Deliciously Low FODMAP
Inspire yourself with hundreds of delicious low FODMAP recipes, tips, and tools, and enjoy the abundance that is yours even when you have IBS.
Use the buttons and filters to find something specific or browse the complete collection for inspiration.
Discover a treasure trove of recipes with my FREE recipe club! Get new ideas delivered straight to your inbox every week.
Deliciously Low FODMAP is a trademark of IBS Game Changer, LLC
Filter to find Recipes and Tools
More Filtering Options
- All 703
- Appetizer 48
- BBQ 46
- Bowl 32
- Breakfast 58
- Cocktails 13
- Collection 1 58
- Collection 10 27
- Collection 11 30
- Collection 12 27
- Collection 13 31
- Collection 14 29
- Collection 15 31
- Collection 16 34
- Collection 17 31
- Collection 18 33
- Collection 19 36
- Collection 2 32
- Collection 20 33
- Collection 21 33
- Collection 22 26
- Collection 3 28
- Collection 4 29
- Collection 5 30
- Collection 6 32
- Collection 7 31
- Collection 8 31
- Collection 9 32
- Condiments 6
- Crock Pot 4
- Dessert 105
- Diabetes Game Changer Exception Protocol Contains Alcohol 11
- Diabetes Game Changer Exception Protocol Contains Flour 106
- Diabetes Game Changer Exception Protocol Contains Flour AND Sugar 76
- Diabetes Game Changer Exception Protocol Contains Sugar 46
- Diabetes Game Changer First Four Weeks 350
- Dinner 318
- Drink 7
- Free Guide 17
- Gluten-free 568
- Gut Microbiome 2
- Guthealth 3
- Holidays 63
- IBS Triggers 4
- Keto Friendly 111
- Lactose-Free 171
- Low FODMAP Diet 689
- Low Net Carb 125
- Low Net Starch 103
- Low Starch 106
Halloween Candy Guide (What’s Low FODMAP and What’s Not)
What you need to know about eating Halloween candy
This time of year Halloween candy is everywhere you look. At work, at parties, at the checkout counter in your favorite store, even at the bank! And it’s tempting to enjoy snacking on a piece or two every place you go.
And let’s face it, at some point, you’re going to want to eat some Halloween candy!
If you are following a low FODMAP diet and Halloween is here. What do you do?
Instead of diving in and eating all of it with wild abandon, how about you do a little learning and planning so you don’t end up feeling terrible?!
Here are three rules to live by:
Don’t eat the candy at all those places I mentioned. You’ll just be stuffing it in your mouth because it’s there. Save your candy-eating for a time you can eat something you particularly like and you can take time to enjoy it.
Read the list below and stick to the low(er) FODMAP candies in the serving sizes recommended.
When you’re finished handing out candy to all the little neighborhood ghouls and goblins, toss it out or donate it. Don’t keep it around the house to “munch on” for days or weeks to come.
Keep it special. Keep it planned. And keep it to a minimum!
This list is excerpted from this post by FODMAP Every Day
Low(er) and High FODMAP Halloween Candy List
For the purposes of this list we are dealing with sweet candies and we feel fairly confident that no natural flavors were derived from onion or garlic, so a few of the candies listed below in the approved columns do contain natural flavors.
If you go rogue and start eating garlic jelly beans (yes, those are a thing), then all bets are off! Don’t do it.
Any candies that clearly list high FODMAP ingredients are on the high FODMAP list.
If you have a history with a particular ingredient, pay attention to your well-earned self-knowledge and stay away.
Serving Size Recommendations
Serving size recommendations are made by Vanessa Cobarrubia RDN as a guide and are based on the Monash University low FODMAP Diet App recommendations for serving sizes for individual ingredients.
As is always the case – we are not offering medical advice and you should always confer with your medical and healthcare team to ensure that you are following guidelines appropriate for your individual body’s needs.
Candy lists are below for your reference. See each list by clicking on the “+” sign to the right.
-
These are the candies we recommend (in alphabetical order by candy name) – in moderation, of course.
Atomic Fireballs: Practice moderation. Maybe 3 per serving.
Boston Baked Beans: Maximum 20 to 25 per serving.
Butterfingers: #7 on many favorite lists. These have some FODMAPs, but they are listed as less than 1% on the label. Start off with half a full-size bar or 1 to 2 fun size bars, or the equivalent of 3 to 4 bites.
Circus Peanuts: Practice moderation. Maybe 4 pieces max. Some say these are the most hated candy – but someone is eating them!
Conversation Hearts: Maybe 6 to 8 pieces max.
Dove Promises Silky Smooth Dark: Limit to 3 pieces (24 g total).
Dum Dums (lollipops): Limit to 4 to 5.
Haribo Gummi Bears: Limit to 15 gummi bears.
Haribo Sour Goldbears: Limit to 15 gummi bears.
Jolly Ranchers: Limit to 3 to 4.
Junior Mints: Limit to 12 mini mints.
Justin’s Dark Chocolate Peanut Butter Cups: Limit to 1 peanut butter cup (20 g) and increase to 2 peanut butter cups (if desired) based on personal tolerance.
Justin’s Milk Chocolate Peanut Butter Cups: There are no additional milk solids, milk, or lactose added in ingredients outside of the milk chocolate. Limiting to 1 peanut butter cup should keep milk chocolate in safe range.
Laffy Taffy: Limit to 3 mini pieces.
Lifesavers Peppermint and Wint-O-Green: Limit to 6
Marshmallows: Exclude any with high fructose corn syrup, inulin or other high FODMAP ingredients: For standard size limit to 4 to 5.
Mounds: Limit to ½ of a full size bar or 1 to 2 snack size bars.
Mr. Goodbar: Limit to ¼ of a full size bar or 1 fun size.
NECCO Wafers: Limit to 10 to 15 wafers.
Nerds: #6 on many lists. Limit to about 1 ½ tablespoons.
Peeps: These are marshmallows; see above. Limit to 3 to 4 peeps.
Reese’s Pieces: Limit to 20 to 25 pieces.
Skittles: #9 on many favorite lists. Limit to 15 to 20 skittles.
Smarties: Limit to 2 rolls.
Sno-Caps: Limit to 1 to 2 tablespoons.
Sour Patch Kids: #8 on many favorite lists. Limit to 6 to 8 pieces.
Swedish Fish: Limit to 2 to 3 pieces.
Sweet Tarts: Limit to 6 to 8 pieces.
-
We recommend that you do not eat these candies. Or, at least know what you are getting into.
Kit Kat: #4 on many favorite lists. Contain wheat flour, lactose, and dairy
Milk Duds: These are milk chocolate based, which is allowed in .5 ounce/15 g amounts, but also contain multiple milk products
Milky Way: These are milk chocolate based, which is allowed in .5 ounce/15 g amounts, but also contain additional milk products, lactose, and malted barley which is untested by Monash
Starbursts: Contain fruit juice concentrates, including apple.
Tootsie Rolls: Contain condensed skim milk and additional whey.
Twix: #3 on many favorite lists. Contain wheat flour, lactose, and dairy
-
For this category, Vanessa recommends trying a small piece to assess your own tolerances. Note that many of these come in “minis”, which might be a great place to start.
Almond Joy: These list milk products multiple times and we cannot be sure of the amount of lactose.
Dove Promises Silky Smooth Milk: These list milk products multiple times and we cannot be sure of the amount of lactose.
Heath Bar: These list milk products multiple times and we cannot be sure of the amount of lactose.
Hershey Bar: #10 on many favorite lists. These list milk products multiple times and we cannot be sure of the amount of lactose.
M & M’s: #5 on many favorite lists. We cannot be sure of lactose content. Try a few.
Mars Bar: These list milk products multiple times and we cannot be sure of the amount of lactose; also lists barley malt.
Nestlés Crunch: These list milk products multiple times and we cannot be sure of the amount of lactose; also lists barley malt.
Reese’s Peanut Butter Cups: #1 on many favorite lists. These list milk products multiple times and we cannot be sure of the amount of lactose.
Skor: These list milk products multiple times and we cannot be sure of the amount of lactose.
Snickers Bar: #2 on many favorite lists. These list milk products multiple times and we cannot be sure of the amount of lactose.
Three Musketeers: These list milk products multiple times and we cannot be sure of the amount of lactose.
Twizzlers: Contain wheat flour
More Deliciously Low FODMAP™ tips & tools
Exploring Metabolic Health: A Special Feature for Metabolic Health Day
20 Minutes prep • 25 Minutes cook • Low FODMAP • Serves 4
Metabolic health is a vital aspect of our overall well-being, yet it often remains overlooked. In recognition of Metabolic Health Day (October 10), in partnership with my sister, Sarah Aitken, RN, MS, WHNP/FNP, NBC-HWC, I’m delving into this crucial topic and addressing some of the most common questions:
What exactly is metabolic health?
Why is it so significant for our overall health?
Can you take steps to improve your metabolic health?
How is blood sugar interconnected with metabolic well-being?
Is it possible to gain insights into your metabolic health by utilizing continuous glucose monitoring?
And perhaps most importantly, can you reverse the consequences of years of neglecting your metabolic health?
Read on to discover the answers to these questions and gain a deeper understanding of the importance of metabolic health in our lives.
Curious about metabolic health? Wondering why it's essential? Ready to take charge of your well-being? You're not alone. Clients often ask these very questions, and the answers can pave the way to better health.
Understanding Metabolic Health
Metabolism fuels your body by converting the food you eat into energy for your cells. Optimal metabolic health ensures that these processes run smoothly. Metabolic health can be assessed through five key markers:
Blood sugar
Triglycerides
HDL (High-Density Lipoprotein)
Blood pressure
Waist circumference
If you're medication-free for these issues and these markers fall within the recommended ranges, your metabolic health is in excellent shape. But there's a sixth marker that's just as important – how you feel. When your metabolic health is on point, you feel good.
The Significance of Metabolic Health
Is metabolic health crucial? Absolutely! If you have three or more "worrisome" markers, you're at risk for diabetes, stroke, Alzheimer's, and heart disease. In fact, these markers can be used to predict or signify heart disease and likely prediabetes or diabetes.
A surplus of glucose in your bloodstream triggers oxidative stress and glycation. Poor metabolic health can lead to:
Low energy or energy fluctuations
Mental fog
Body pain
Fluid retention
Poor exercise stamina
Weight challenges
Widely varying moods
Skin issues
Fertility problems
Low libido or sexual issues
Susceptibility to infections
Improving Your Metabolic Health
Can you improve your metabolic health? Yes, you can! In the past, metabolic health was more of a given due to lifestyle and dietary choices. But as processed foods and snacking have become the norm, metabolic health has declined. In 2019, 88% of North Americans were deemed metabolically unhealthy. That means only 12% of us are metabolically healthy!
You can improve your metabolic health, often called metabolic fitness, by making daily choices that support your metabolic processes. Your diet, meal timing, sleep, stress management, physical activity, and more all play roles in this dynamic state of well-being. It's not an on/off switch; it's a daily continuum determined by your choices.
The Connection Between Blood Sugar and Metabolic Health
Glucose from your food is your cells' fuel. Insulin helps cells use glucose, but when cells aren't hungry for fuel due to frequent eating or highly processed foods, they become insulin resistant. This protective response keeps glucose out of cells, preventing them from overloading. When your blood sugar rises, it's a signal your cells are resisting insulin.
Can you tell something about your metabolic health by wearing a continuous glucose monitor (CGM)?
Absolutely! The glucose pattern of someone in poor metabolic health looks erratic, a roller coaster of variability.
They will likely see higher glucose peaks after eating high-starch foods. Their glucose may remain elevated for two or three hours after a meal or go up and down for several hours after eating. Morning glucose may be high, and/or the average glucose can be high.
Reversing the Damage of Poor Metabolic Health
Can you reverse the damage done by years of poor metabolic health? The answer is yes and no. Your organs and systems adapt to defend against glucose toxicity. This defensive mode can lead to various issues.
You can halt and even reverse some of this damage by:
Reducing the pressure on your liver, cardiovascular system, and pancreas
Lowering inflammation
Allowing for cellular cleanout
There's hope for a healthier future, and you have the power to optimize your metabolic health through daily choices.
Armed with this knowledge, you may feel you need help to make some changes to address your Metabolic Health. That’s where health coaching comes into play. If you have IBS and Metabolic Health concerns, learn about my program and set up a free consult with me and we can talk about how to tackle your issues! If you do not have IBS but you have pre-diabetes, weight management issues, or other metabolic health imbalances, then head on over to my sister site, Diabetes Game Changer. It might be just what you need to prepare yourself to have the best new year ever.
Here's to your best health and a thriving, resilient body.
Have a question you’d like to have answered? Email me at hello@ibsgamechanger.com
More Deliciously Low FODMAP™ tips and tools
Understanding Constipation: A Must for IBS Sufferers
Constipation: What is it? What are some common myths about it? What can you do about it?
What is it? What are some common myths about it? What can you do about it? And why are you looking at a picture of coffee?
For those of us with IBS, constipation is an important symptom to understand. If you're experiencing new or worsening constipation, seeking a gastroenterologist's evaluation, including a colonoscopy, is essential to rule out any underlying causes other than IBS. In this article written by my sister, Sarah Aitken, RN, MS, WHNP/FNP, NBC-HWC, for her Diabetes Game Changer Program, you'll find answers to most of the questions you might have about constipation.
Here’s the “Bottom” Line:
Whether you have IBS-C, IBS-D, or a combination of the two, IBS can manifest as constipation intermittently or all the time. I encourage you to read the full article for all the details.
Constipation has little to do with how often you poop and everything to do with how easy and comfortable your GI tract feels
Suffering from constipation does not mean you have an unhealthy diet
Hydration matters a lot
Moving your body matters, especially after meals
A regular and predictable eating routine helps
Medications could be the cause, so check them out with your provider
Increasing your intake of soluble fiber and avoiding processed foods might be all you need to do to fix the problem!
Still having issues and need customized and personalized support? Sign up for my IBS Game Changer Program and we can work together to get your gut on track.
More Deliciously Low FODMAP™ tips and tools
Olive Oil, Which One Should I Use?
Read the full article to know which oil to choose for your recipes.
The wide world of olive oil can be confusing! But essentially there are three main kinds of olive oil, and they all have their pros and cons based on their ingredients and the methods used to extract the oil. My top pick? Extra-Virgin Olive Oil (EVOO) whenever possible. It’s healthy and delicious, and using it liberally can help keep you in tip-top health while delivering highly satisfying flavor in your recipes. You will notice I use a LOT of olive oil in my recipes. I don’t always label it EVOO, but I should!
Thanks to my amazing sister, Sarah Aitken, RN, MS, WHNP/FNP, NBC-HWC, I’m sharing this article she recently published for her Diabetes Game Changer newsletter. Sign up here to get Sarah’s Monday Motivation email newsletter, it’s great!
What do you know about Olive Oil? It’s really interesting!
Olive oil is packed with a variety of polyphenols, which have powerful antioxidant properties.
Diets high in olive oil are associated with reduced inflammation, improved heart, brain, and gut health, and more. In addition, olive oil contains phytosterols, which are bioactive compounds associated with reduced cholesterol and even a reduction in the incidence of some types of cancer.
Olive oil differs from other oils, such as canola, vegetable and soybean oil in a few very key ways. The seed oils are extracted and refined using very high heat and chemicals, resulting in less flavor and a destruction of the health benefits that may be included in unrefined oils. The base foods in these oils afford few, if any, health benefits and may even have negative health consequences (more on the topic of seed oils to come!)
Olive oil is one of our oldest foods - anthropologists have found evidence that humans made olive oil thousands of years ago using stone mills.
Read the full article to know which oil to choose for your recipes.
More Deliciously Low FODMAP™ tips and tools recipes
Tips for Navigating the Grocery Store Low FODMAP Style
A step-by-step guide to assist you in getting through the grocery store and coming out with all the low-FODMAP foods and ingredients you need.
Figuring out how to navigate a low-FODMAP diet can be challenging on its own. When you add the task of navigating the grocery store to find low-FODMAP foods and ingredients for enjoyable family meals, it can feel overwhelming and discouraging even before you’ve set foot in the store! To simplify this process, I've created a step-by-step guide to assist you in getting through the grocery store and coming out with all the low-FODMAP foods and ingredients you need.
Low FODMAP Grocery Shopping Made Easy
Educate Yourself: Familiarize yourself with the list of high and low FODMAP foods. You can use the Monash app or the Spoonful app for packaged foods, and you can use my food and shopping lists for easy/quick planning and buying.
Plan Your Meals: Before you go shopping, plan your meals and make a shopping list based on my low FODMAP recipes and meal plans. This will help you stay focused and avoid purchasing non-compliant foods.
Read Food Labels: When shopping, carefully read food labels for ingredients that are high in FODMAPs. Look out for ingredients like wheat, garlic, onion, high-fructose corn syrup, and artificial sweeteners. Avoid foods that contain these ingredients. Use the Spoonful app to scan barcodes and help you quickly assess FODMAP ingredients to watch for.
Stick to Whole Foods: The safest way to ensure you're getting low FODMAP ingredients is to focus on whole, unprocessed foods. Fresh fruits and vegetables, lean meats, fish, eggs, lactose-free dairy, rice, quinoa, and some gluten-free grains like oats are generally safe options.
Check for Certified Low FODMAP Products: Some brands now offer certified low FODMAP products. Look for the "Certified Low FODMAP" logo on the packaging, as this indicates that the product has been tested and approved as suitable for a low FODMAP diet. Some examples include Smoke N Sanity seasonings, salsas, and sauces; Fody Foods products, Green Valley and Good lactose-free dairy products, and others.
Avoid Onions and Garlic: Onions and garlic are common high FODMAP ingredients used in many processed foods and condiments. Instead, look for garlic-infused oils (the oil contains the flavor but not the FODMAPs) or use onion and garlic substitutes like garlic-infused oil or just the green parts of green onions, leeks, and spring onions.
Shop the Perimeter: In many grocery stores, the outside aisles of the store are where you'll find fresh produce, meats, dairy, and other whole foods. These are generally safer choices for a low FODMAP diet than all the processed foods on the inside aisles.
Beware of Hidden FODMAPs: Some foods that seem healthy may contain hidden FODMAPs. For example, certain fruits and vegetables in dried or canned forms, some gluten-free products, and certain sauces or marinades can contain high FODMAP ingredients.
Experiment and Keep a Food Diary: Everyone's tolerance to FODMAPs is different. After shopping for low FODMAP ingredients, be prepared to experiment with portion sizes and combinations of foods to determine what works best for your individual needs. Keeping a food diary can be helpful for tracking your symptoms and identifying trigger foods. The shopping lists linked in this article are excerpted from the journal I provide my coaching clients to track not only food and drink, but also exercise, stress level, bowel movements, and more.
Remember that while a low FODMAP diet can be beneficial for managing IBS symptoms, there’s more to it than that. Working with a healthcare professional who specializes in gastrointestinal health can be a real game changer. That’s why I created my 8-week program to provide just the right amount of guidance, education, and support to go from unpredictable and uncomfortable to predictable, comfortable, and in the driver’s seat! Take a look at the program here and read some of the success stories from program graduates.
Link note: This post may contain affiliate links for you to easily purchase items that are linked. I may earn a small commission from qualifying purchases but none of this costs you a thing so feel free to use the links! In addition, for some items, I have provided a special discount code for IBS Game Changers so be sure to use the code when you purchase an item to get the discount that has been arranged just for you.
More Deliciously Low FODMAP™ Tips and Tools
The Delicious Dimension: Exploring the Visual and Textural Joys of a Restricted Diet
While the nutritional content of food takes center stage, the way food looks and feels should not be underestimated.
When you’re limiting the selection of foods you eat for any reason, it’s important that the foods you do eat are as appealing and delicious as possible. That includes what your food LOOKS like and what it FEELS like when you eat it! Embarking on a restricted diet can be a challenging journey, often requiring meticulous attention to what you eat. While the nutritional content of food takes center stage, the way food looks and feels should not be underestimated. In this post, I’m digging into the significance of considering the aesthetics and textures of food when following a restricted diet and why this aspect matters for our overall well-being. I’ve included lots of links to delicious low-FODMAP recipes you can try when you’re ready to experience the many amazing things you can eat when following a low-FODMAP diet.
The Power of Presentation
A Feast for the Eyes: The old adage "we eat with our eyes first" holds true, especially for those on restricted diets. The visual appeal of food plays a crucial role in anticipation, satisfaction, and even the desire to consume the meal. When faced with dietary limitations, crafting visually appealing dishes can make each meal a delightful experience. Taking the time to chop some fresh herbs, grate some extra-flavorful cheese, or drizzle a little olive oil on the final dish can make all the difference. Try this Chicken Cobb Salad or Spring Roll Salad with Peanut dressing in my recipe club for example, or Better Than Takeout Sesame Chicken on my blog.
Emotional Fulfillment: Restricted diets can evoke feelings of deprivation and monotony. By putting effort into the visual presentation of meals, we transform our eating experience from a mere necessity to an emotionally satisfying ritual. A colorful and well-arranged plate can boost mood and elevate the overall enjoyment of the meal. Try my Super Simple Chocolate Lava Cakes or my Mushroom Gruyere Savory Bread Pudding, for example or any of the soup recipes in my recipe club.
The Crucial Role of Texture
A Multisensory Experience: Texture influences our perception of food more than we realize. The crunch of a fresh salad or the creaminess of mashed potatoes engages our senses, enhancing the dining experience beyond taste alone. This multisensory engagement becomes especially significant on restricted diets where the range of foods may be limited. Try my Crisp and Crunchy Chicken Salad, or my One Pan Thai Peanut Chicken and Veggies for example.
Appetite Stimulation: Texture can influence our appetite as well as our sense of satiation. Foods with varying textures stimulate our taste buds and appetite, making us more likely to enjoy and feel satisfied with a meal. For those adhering to specific dietary restrictions, incorporating diverse textures can make each bite more enticing. Try my Vegetable Chicken Stew, or my Chinese New Year Chicken Salad for example.
Mimicking Familiar Foods: On restricted diets, finding alternatives to favorite foods can be challenging. Texture can play a crucial role in replicating the experience of familiar meals. For example, creating a gluten-free pizza crust with a satisfying array of toppings can, not only mimic the texture of traditional pizza, but you might just find you like it even better than the original! This sameness with your old standards can provide a sense of comfort and normalcy. Check out this amazing Rosemary Mushroom Flatbread, or this BBQ Chicken Pizza with Bacon and Pineapple, or my Chocolate Cake with Umami Chocolate Frosting, in my recipe club for inspiration!
Expanding Culinary Creativity: Exploring new textures within the confines of a restricted diet can foster culinary creativity. Discovering how to use ingredients like nuts, seeds, and alternative flours to create crunchy crusts, velvety sauces, or chewy snacks can turn dietary limitations into an opportunity for innovation. In my recipes, I do my best to incorporate as much variety as possible—especially when it comes to plants as they play a vital role in keeping our gut biome healthy. Try my Umami Chicken and Butternut Squash Ramen, or my One Pan Chicken Arroz Caldo, for example.
Summing it all up
As we all experience our own IBS journey and the Low FODMAP diet that often accompanies that journey, keep in mind that food is not just sustenance—it's a sensory experience. The way food looks, feels, and engages our senses can significantly impact our relationship with our meals. By embracing the power of presentation and texture, you can infuse joy, anticipation, and a deeper connection with your meals. Crafting visually appealing dishes and experimenting with diverse textures can turn the challenge of eating a restricted diet into an opportunity to explore new horizons. So, let's celebrate the beauty and diversity of food, even within the boundaries of our dietary restrictions. After all, savoring a meal is not just about nourishment; it's about relishing life's sensory pleasures.
Have a question you’d like to have answered? Email me at hello@ibsgamechanger.com
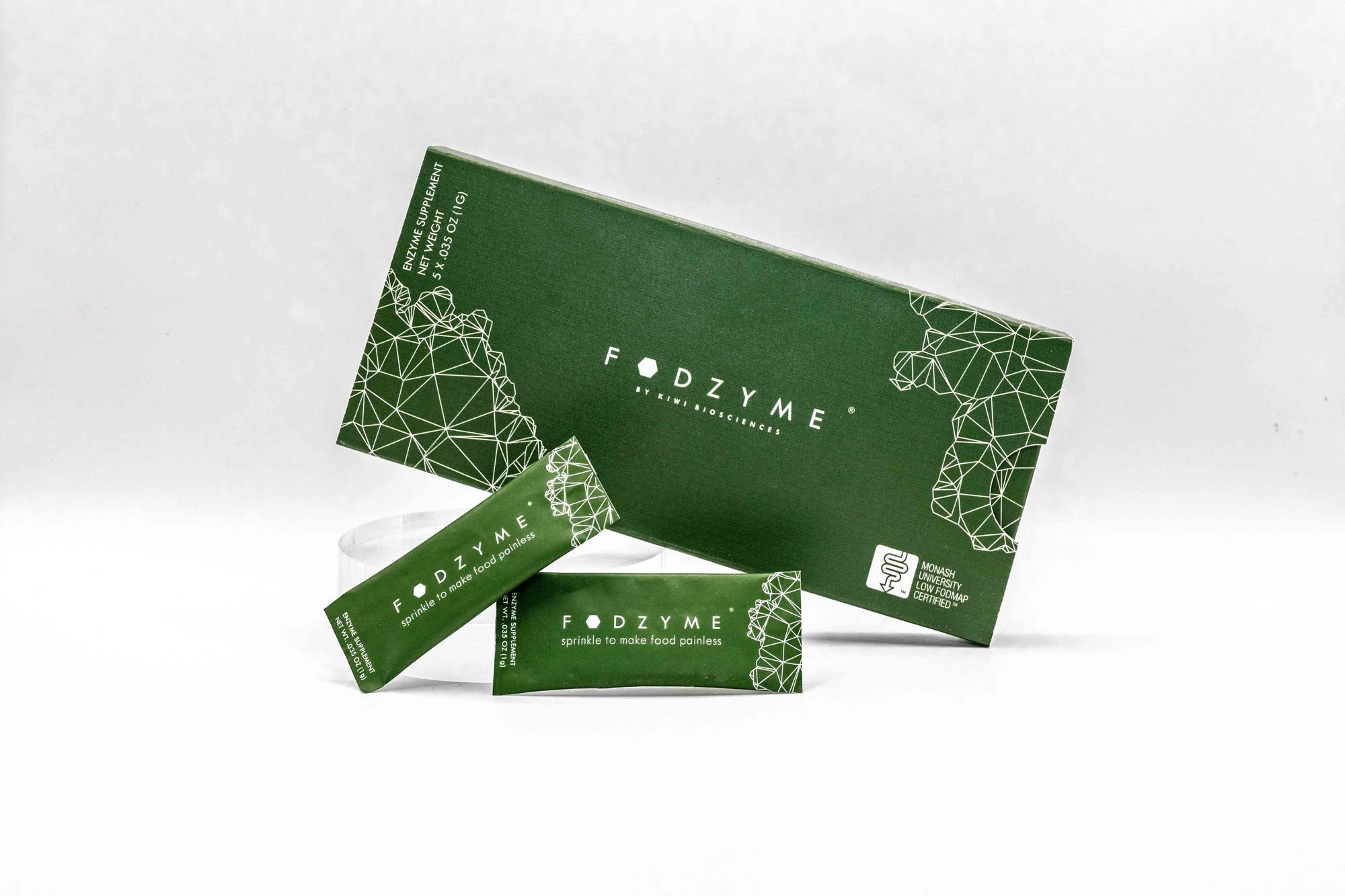
Haven’t tried FODZYME yet? Get a free sample!
If you are based in the United States and have never tried FODZYME before, you can get a free sample of FODZYME.
Not long ago, I wrote a full post about FODZYME. You can find that article here. In it, I asked, what if you (with IBS) could eat garlic, onions, pizza, and even ice cream without GI consequences? That would be a game-changer.
Now, you can try FODZYME for free!
If you are based in the United States and have never tried FODZYME, you can request a free sample of FODZYME using the button above. Complete and submit the form and they will send you your free sample right away.
Does it work and how does it work?
As with everything else I recommend, I tried it myself. And it worked for me. Does that mean it will work for you too? The only way to find out is to give it a try yourself. Each of us has a different FODMAP sensitivity profile so we may each have a different experience with a product like FODZYME. But seriously, what do you have to lose?
We are all likely familiar with Lactaid the enzyme that breaks down lactose. FODZYME is similar in concept but, as a powder rather than a pill, FODZYME may have an advantage that allows it to work much better. And, it’s the world's first enzyme supplement that breaks down FODMAPs.
Adding FODZYME directly to the food you are eating (vs taking a pill with the same enzymes in it) has been proven to be the most effective way to activate these enzymes. Once ingested and activated these enzymes serve to reduce or eliminate the painful reaction that comes with eating foods that are high in the FODMAPs fructan, GOS, and/or lactose. And soon, the formulation will cover the Polyols too.
Need a refresher on what foods contain Fructan, GOS, and lactose?
Fructan and GOS Examples: Almonds, Artichoke, Baby spinach, Banana, Beans, Beetroot, Blueberries, Broccoli, Brussels sprouts, Cabbage (red and savoy), Cashews, Chickpeas, Cranberries, Dates, Figs, Garlic, Grapefruit, Leek, Lentils, Onion, Peas, Pistachios, Pomegranate, Raspberries, Roma Tomatoes, Scallion, Shallots, Silken tofu, Wheat, and Zucchini.
High Lactose Examples: Buttermilk, Cheese, Queso Fresco, Cottage cheese, Cream, Creamy cheeses, Custard, Goats cheese, Haloumi, Ice-cream, Kefir, Milk, Paneer, Quark cheese, Ricotta cheese, Sour cream, Yogurt.
Already tried FODZYME and want to buy more?
Click the button below to buy more so you can enjoy the foods you love without the GI consequences.
Use my discount code IBSGC15 for a 15% discount.
More Deliciously Low FODMAP™ Tips and Tools
Curious about Keto and using the Keto Diet to Manage IBS Symptoms?
A ketogenic diet could be one pathway to relief for some of us with IBS
Irritable Bowel Syndrome (IBS) affects millions of people worldwide and if you are reading this, it’s likely you are one of those people. Unfortunately, there’s no one-size-fits-all solution for managing IBS, which is why I am constantly learning and researching new possibilities to share with you. Recently, I attended a conference for Metabolic Health Practitioners and much of the data presented led me to conclude a ketogenic diet could be one pathway to relief for some of us with IBS. In this blog post, I am sharing how the keto diet can potentially help control your IBS symptoms, and what the keto diet is, along with some practical tips for getting started on a keto diet.
The Basics of the Keto Diet
The ketogenic diet is higher in healthy fats, and lower in carbohydrates which is designed to shift the body into a state of ketosis, where it burns fat for fuel instead of carbohydrates. This metabolic shift can impact various aspects of health, including mental alertness and concentration, getting rid of excess weight, and managing IBS symptoms. Because all FODMAPs are carbohydrates, it stands to reason a low-carbohydrate diet will reduce your IBS symptoms. For some people with IBS, trying to understand FODMAPs and what you can and cannot eat is a huge challenge. The keto diet may help simplify things to the point that real relief from IBS symptoms can be achieved and maintained without having to focus so much on the potentially overwhelming world of FODMAPs.
The Potential Benefits for People With IBS
Reduced Carbohydrate Intake: This is the primary pathway to relief because we know all FODMAPs are carbohydrates and FODMAPs can trigger IBS symptoms in most people with IBS. The keto diet drastically limits carb intake, potentially reducing exposure to FODMAPs and eliminating most symptom triggers.
Improved Gut Microbiome: As I’ve mentioned before, there’s emerging research that points to a connection between the gut microbiome and IBS symptoms. The keto diet might positively influence the gut microbiome composition, which could alleviate IBS symptoms.
Stabilized Blood Sugar Levels: Fluctuating blood sugar levels can contribute to IBS symptoms. The keto diet's focus on fats and proteins can help stabilize blood sugar, potentially reducing the symptoms that are related to excess sugar.
Implementing the Keto Diet for IBS Management
Before making dietary changes, it’s always a good idea to consult your own healthcare provider, especially if you have other underlying health conditions. They can guide you on whether the keto diet is suitable for you.
Once you get the go-ahead, ease into the keto diet slowly to allow your body to adapt. Drastic changes can sometimes trigger digestive discomfort.
When eating a keto diet, opt for low-FODMAP foods within the keto framework. Examples include meats, fish, eggs, non-starchy vegetables, and certain nuts and seeds. Keep in mind, you are taking carbs out and adding fats in. If you have questions about the FODMAPs in any food, I recommend using the Monash University FODMAP app. It’s the gold standard when it comes to food and FODMAPs.
Keep yourself hydrated. This, of course, applies to all diets but in particular, the keto diet that can cause increased water and electrolyte loss. If you have trouble maintaining your electrolyte balance as a result of fluid loss, I recommend using Trace Minerals 40,000 Volts drops (up to 1 teaspoon per day) to maintain electrolyte balance without adding sugar or other FODMAP-containing ingredients to your diet.
While the keto diet is low in carbs, incorporating low-carb, non-starchy vegetables can provide essential fiber to support gut health. (If you find you need more fiber, I recommend adding up to one scoop of Paleo Fiber Resistant Starch Fiber to your daily routine.)
Finally, mindful eating is more important than you might think no matter what diet you may be on. Pay attention to serving sizes and listen to your body's cues for fullness and satiation. Overeating on anything, even on keto-friendly foods, can exacerbate IBS symptoms.
Getting Started
Getting started on a keto diet requires some planning and preparation. Here's a step-by-step guide to help you get started:
Review the list of basic keto-friendly foods below.
Stock your kitchen. Clean out your pantry and stock up on keto-friendly ingredients. Focus on foods like avocados, olive oil, nuts, seeds, eggs, fatty fish, and non-starchy vegetables. Having these items readily available will make cooking keto meals much easier.
Plan your meals. Start by creating a meal plan that includes a variety of keto-friendly foods. Incorporate low-carb vegetables, lean proteins, healthy fats, and small portions of low FODMAP options. Planning your meals ahead of time will help you stick to the diet and avoid last-minute temptations. I have lots of low-FODMAP Keto-friendly recipes in my recipe club. Here’s a filtered view for you to find many of them.
Listen to your body. Every individual's response to the keto diet is unique. Pay attention to how your body reacts, and adjust your dietary choices accordingly. If you encounter persistent discomfort or adverse effects, consult your healthcare provider.
Remember, the keto diet isn't suitable for everyone, and its long-term effects are still being researched. It's important to prioritize a balanced, nutrient-dense diet that meets your individual needs and health goals. If the keto diet doesn't align with your preferences or health considerations, there are numerous other dietary strategies to explore in managing IBS symptoms. Always choose an approach that you enjoy and you can stick with or you won’t succeed.
So what do you eat on a keto diet?
On a keto diet, you'll primarily focus on consuming foods that are high in healthy fats, moderate in protein, and low in carbohydrates. Here's a list of basic foods that are typically included in a keto diet:
Healthy Fats:
Avocado (keep to 1/8 per sitting for low FODMAP) and avocado oil
Coconut oil and coconut products
Olive oil
Butter and ghee
Nuts and seeds (e.g., almonds, walnuts, chia seeds)
Fatty fish (e.g., salmon, mackerel)
Cheese (in moderation)
Heavy cream
Protein Sources:
Lean meats (e.g., chicken, turkey, beef, pork)
Fatty cuts of meat (e.g., bacon and sausage but watch for onions/garlic in the ingredients)
Eggs
Fish and seafood
Tofu (firm tofu is low FODMAP) and tempeh (for vegetarians)
Low-Carb Vegetables:
Leafy greens (e.g., spinach, kale, lettuce)
Cruciferous vegetables (e.g., broccoli tops are low FODMAP, and Arugula too)
Zucchini
Bell peppers
Cucumber
Berries (in Moderation):
Strawberries
Blueberries
Raspberries
Dairy Alternatives (if you don’t tolerate dairy well):
Unsweetened almond milk, coconut milk, or other plant-based milk (but watch for FODMAP ingredients)
Dairy-free cheese alternatives (check labels for carbohydrate content)
Herbs, Spices, and Condiments:
Herbs and spices (e.g., basil, oregano, etc.)
Salt and pepper
Vinegar
Mustard
Hot sauce
Beverages:
Water
Herbal tea (without added sugar)
Black coffee (decaf is best for those with IBS and in moderation)
Summing it up
The keto diet holds promise as a potential tool for managing IBS symptoms. However, it's crucial to remember that everyone's body responds differently to dietary changes. What works for one person might not work for another. The keto diet should be undertaken with careful consideration, ideally under the guidance of your healthcare provider. It's also important to continue exploring other IBS management strategies, such as exercise, stress reduction techniques, and identifying specific trigger foods. Using this comprehensive approach, you can work towards reducing the impact of IBS on your quality of life. If you want expert guidance and coaching to support your health journey, check out my complete coaching program here. I would love to help you!
Have a question you’d like to have answered? Email me at hello@ibsgamechanger.com
More Deliciously Low FODMAP™ Keto-friendly recipes
Delicious Low FODMAP Beef Sticks and Jerky from Good Fod Foods
Thanks to our friends at Good Fod Foods you can now have delicious Beef Sticks and Jerky in a variety of flavors that you can keep on hand for a quick snack or light lunch on the go.
When you have Irritable Bowel Syndrome (IBS) sometimes it’s hard to find a good “car snack” or on-the-go food for hiking or backpacking that you can count on for flavor, nutrition, and shelf stability. Or, you’re just trying to get more protein in your everyday low FODMAP diet without adding a bunch of calories. Thanks to our friends at Good Fod Foods you can now have delicious Beef Sticks and Jerky in a variety of flavors that you can keep on hand for a quick snack or light lunch on the go. The beef sticks are tender, flavorful, and easy to chew. The jerky is just that—jerky! Exactly the way you want it to be and all the flavors are delicious. As usual, I have arranged a 15% discount (IBSGC15) just for you. In fact, if you click the image or button below to start shopping, the discount will be automatically applied to your cart at checkout!
The Good Fod Foods family dealt with sensitive stomachs for a while before they tried a low-FODMAP diet. They felt better and they realized it was hard to find nutritious, shelf-stable low-FODMAP snacks. So, they made some to share! I tried them all and I can personally say they are delicious.
Give them a try with the IBS Game Changer 15% Discount.
More Deliciously Low FODMAP™ tips & tools
What if you (with IBS) could eat garlic, onions, pizza, and even ice cream without GI consequences?
How can I eat fructan, GOS, and lactose when on a low FODMAP diet? FODZYME might help!
That would be a game-changer.
If you have Irritable Bowel Syndrome (IBS) and it has been recommended that you follow a low FODMAP diet you may have a lot more questions than you do answers. And you may feel completely baffled by all of the information out there and all of the various recommendations and guidelines you “should” follow.
How often have you said why can’t I just eat like everyone else does? Why does food have to make me feel sick? Where’s the magic fairy dust that I can sprinkle on my food and turn it into something I can eat without consequences?
That magic fairy dust might just be here in the form of FODZYME®
Those of you who know me, or who have worked with me as an IBS coach, know I’m not a fan of supplements and pills. But, there’s a time and a place for everything. And this product may be a game changer for many of you when you’re traveling, eating out, or choosing to eat a food you know you are sensitive to.
I wanted to learn more, so I sat down with Harvard-educated co-founder David Hachuel, to learn more about FODZYME and how it works.
FODZYME is made by Kiwi Biosciences, “a human-centered biotech company developing elegant solutions for extraordinary gut relief.” The current FODZYME formula is a highly-specific enzyme blend designed to target the FODMAPs fructan, galactooligosaccharides (GOS), and lactose.
FODZYME is a blend of digestive enzymes that has been lab tested and certified low FODMAP by Monash University, which means the ingredients in FODZYME are considered low FODMAP.
Does it work and how does it work?
As with everything else I recommend, I tried it myself. And it worked for me. Does that mean it will work for you too? The only way to find out is to give it a try yourself. Each of us has a different FODMAP sensitivity profile so we may each have a different experience with a product like FODZYME. But seriously, what do you have to lose?
We are all likely familiar with Lactaid the enzyme that breaks down lactose. FODZYME is similar in concept but, as David explained, as a powder rather than a pill, FODZYME has an advantage and works much better. And, it’s the world's first enzyme supplement that breaks down FODMAPs.
Adding FODZYME directly to the food you are eating (vs taking a pill with the same enzymes in it) has been proven to be the most effective way to activate these enzymes. Once ingested and activated these enzymes serve to reduce or eliminate the painful reaction that comes with eating foods that are high in the FODMAPs fructan, GOS, and/or lactose. And soon, the formulation will cover the Polyols too.
Need a refresher on what foods contain Fructan, GOS, and lactose? Click the expansion arrows below for some prime examples:
-
Examples: Almonds, Artichoke, Baby spinach, Banana, Beans, Beetroot, Blueberries, Broccoli, Brussels sprouts, Cabbage (red and savoy), Cashews, Chickpeas, Cranberries, Dates, Figs, Garlic, Grapefruit, Leek, Lentils, Onion, Peas, Pistachios, Pomegranate, Raspberries, Roma Tomatoes, Scallion, Shallots, Silken tofu, Wheat, and Zucchini
-
Examples: Buttermilk, Cheese, Queso Fresco, Cottage cheese, Cream, Creamy cheeses, Custard, Goats cheese, Haloumi, Ice-cream, Kefir, Milk, Paneer, Quark cheese, Ricotta cheese, Sour cream, and Yogurt
-
Examples: Apple, Apricot, Avocado, Blackberries, Cauliflower, Celery, Cherries, Lychee, Mushrooms, Nectarine, Peach, Pear, Plum, Prune, Sauerkraut, Sweetcorn, Sweet potato
Sound interesting? Want to give it a try? Use the IBS Game Changer discount code for 15% off. What are you waiting for?
More Deliciously Low FODMAP™ tips & tools
Why Eating Fermented Foods Benefits You and Your Gut - And How to Eat More
If someone told you there was a natural, inexpensive, non-prescription way to boost your mood, modulate your weight, and avoid getting sick, I bet you’d be quite interested! Read this post to learn more.
If someone told you there was a natural, inexpensive, non-prescription way to boost your mood, modulate your weight, and avoid getting sick, I bet you’d be quite interested! Well, I’m here to tell you there is! And all you have to do is get a bit of fermented food in your diet each day. Wondering how to pack a peck of pickled peppers into your diet? In this post, I have put together a list of the most common fermented foods and their benefits, including the low FODMAP serving of each.
Eating Fermented Foods:
-
Adding fermented foods to your diet increases the number of beneficial bacteria in your gut. Some of those beneficial bacterial convert to hormones such as Serotonin (the happy hormone) which helps boost your mood. A healthy gut full of beneficial bacteria contributes to and supports your mental health and cognitive function – think improved memory and concentration!
-
Eating fermented foods can increase your antibodies which protect you against invading pathogens naturally improving your immunity.
-
Eating fermented foods can help regulate your hunger hormones, which in turn can help to control your weight. Adding fermented foods to your diet may also help reduce sugar and carbohydrate cravings too!
-
Adding fermented foods to your diet can make the nutrients more bio-available and more digestible so your gut doesn’t have to work so hard to get the most out of what you eat.
-
Adding fermented foods to your diet can help reduce systemic inflammation. Reducing inflammation can help with chronic diseases such as arthritis and cardiovascular disease. It can also help offset inflammatory lifestyle factors such as poor diet, excess caffeine, overconsumption of sugar, certain medications, etc.
Some common fermented foods—and Low FODMAP servings
Yogurt (lactose-free) - Low FODMAP Serving Size: 6 ounces
Yogurt is one of the most popular and common fermented products available today. Be sure to choose organic whenever possible. Also look for natural, and probiotic-rich yogurt for maximum health benefits. And of course, steer clear of the highly sugared yogurt parfaits. Plain lactose-free yogurt with some nuts, homemade granola, or fruit on it is ideal. Vegans (or those who don’t tolerate the whey in milk) can try coconut yogurt made with organic coconut milk fermented with probiotic starter.
Kombucha - Low FODMAP Serving Size: 6 ounces
A very popular fermented tea drink that uses a colony of yeast and bacteria known as a SCOBY (Symbiotic Culture of Bacteria and Yeast). It might not sound very good, but tastes delicious! It can be flavored with different fruits and spices to create a mildly fizzy, gut-loving, highly beneficial, delicious drink. Look for one that doesn’t have added sugar (it will always be fermented with fruit or something that has sugar anyway). My favorite is GT’s Marine Greens which is fermented with Kiwi juice and tea. As it contains some a small amount of caffeine even after fermenting, it’s important to adjust the serving size to your tolerance and have it early in the day!
Kefir (lactose-free) - Low FODMAP Serving Size: 8 ounces (or 1 Tablespoon of traditional Kefir with Lactose)
Milk kefir is a tart, drinkable, natural yogurt. It contains many beneficial probiotics and is high in Vitamin B12, calcium, and magnesium. It can easily be added to smoothies for a simple probiotic boost. Water kefir is just as beneficial and is ideal for vegans. It is made from grains and can be flavored in a similar way to Kombucha.
Apple Cider Vinegar - Low FODMAP Serving Size: 2 Tablespoons
Apple Cider Vinegar (ACV) contains acetic acid which supports the function of probiotics and prebiotics in your gut. It is ideal as a blood sugar balancer and digestive aid. Mix it into salad dressings, soups, and sauces, or add a teaspoon to a glass of warm water before meals to help with digestion. ACV contains important digestive enzymes. Taken before bed, it can have a positive effect on morning fasting blood sugars.
Here’s an article I wrote about taking ACV as a supplement while on a low FODMAP diet.
Sourdough Bread - Low FODMAP Serving Size: 1 Slice (.92 ounces)
The long fermentation process involved in making sourdough bread helps to make nutrients found in the grains, more available for absorption and reduces the antinutrient content that may make digestion difficult. Those with gluten sensitivity, who might usually experience bloating and indigestion when eating regular bread, may have little or no digestive symptoms when eating real sourdough bread. To identify “real” sourdough bread, it must not include commercial yeast or vinegar in the list of ingredients. These are used to create bread that tastes like sourdough but is not actually fermented. If you go to your local bakery, where you’ll find the absolute best sourdough bread, you can ask to confirm it is made in the traditional way with a long period of fermentation.
Miso - Low FODMAP Serving Size: 1 Tablespoon
Miso is a soybean paste that is made from brown rice or barley fermented with a type of fungus called Koji. Traditionally used in Asian recipes, as a base for soup, it’s a great flavor enhancer and probiotic food booster. Try adding it to salad dressings along with apple cider vinegar and to soups and stews. There are multiple varieties (all good!) and you can buy them in most grocery stores. You can also make it yourself (if you don’t mind waiting at least 12 months for it to mature!)
Sauerkraut - Low FODMAP Serving Size: 1 Tablespoon
Traditionally made from white cabbage, it can also be made with red cabbage, fennel, and other vegetables. Sauerkraut is rich in fiber, B vitamins, Vitamin K, and Vitamin C. It’s also an excellent source of trace minerals which are important for blood clotting and healthy bones. Simply add a spoonful of sauerkraut to your salads or soups 3-4 times per week for optimum health benefits.
Sauerkraut is extremely cheap and easy to make. Want to make your own? Here’s an excellent how-to article from which much of this content was derived.
Kimchi - Low FODMAP Serving Size: 1/4 cup (1.66 ounces)
Kimchi is a Korean delicacy dating all the way back to the 7th century. It is a spicy version of sauerkraut that is typically made with Chinese leaves, garlic, ginger, and chilies (so read the ingredients before diving in and look for one without the garlic.) These add potent anti-inflammatory properties as well as antioxidants to the probiotic benefits. It can be added to your next stir-fry or soup for a strong flavor boost.
Tempeh (plain) - Low FODMAP Serving Size: 1 Slice (3.5 ounces)
Tempeh is made from whole fermented soybeans, to create a very dense, cake-like product that contains more probiotics and health benefits than the more well-known soybean-based food, Tofu. It is more textured than tofu, chewier, and much higher in protein. It can be used as a meat substitute. It’s sometimes hard to find plain tempeh so watch for FODMAP ingredients used to flavor the tempeh.
Tofu (firm/drained) - Low FODMAP Serving Size: 1 Cup
Tofu is also made from fermented soybeans and it can easily absorb flavors which makes it very versatile in recipes. It is a great source of protein important for the growth and repair of tissues. It also contains Phyto-estrogen compounds – important for hormone balancing (particularly in menopause). If possible, always choose non-GMO sourced tofu, not the highly processed soy protein isolate you often find in the grocery store. And, for low FODMAP, always use firm tofu (not the silken variety).
Have a question you’d like to have answered? Email me at hello@ibsgamechanger.com
More Deliciously Low FODMAP™ tips and tools
What’s so Great About Olive Oil? Everything!
Which olive oil is best? Extra virgin olive oil (EVOO)? Virgin olive oil? Just straight-up olive oil? Read this article and it will all make sense.
If you’ve been with me for long, you know I use olive oil in just about all of my savory recipes. Why is that? Because it’s delicious, of course, and also because it has some amazing health properties. I buy all my olive oil at a local farmstand. They make their own olive oils, they are always fresh and delicious and they offer many different infused olive oils that are also wonderful. I realize not everyone will have such a bounty in their backyard, so I’m sharing this article, written by my amazing sister Sarah Aitken and featured in her Diabetes Game Changer Program, that will help you navigate the vast array of olive oils on the supermarket shelves so you can buy the one that’s best for you.
Olive oil differs from other oils, such as canola, vegetable, and soybean oil in a few very key ways. These oils are extracted and refined using very high heat and chemicals, resulting in less flavor and destruction of the health benefits that may be included in unrefined oils. But which olive oil is best? Extra virgin olive oil (EVOO)? Virgin olive oil? Just straight-up olive oil?
The wide world of olive oil can be confusing! But essentially there are just 3 main kinds, and they all have their pros and cons based on the ingredients used and the methods of production. My top pic? EVOO whenever possible. It’s healthy AND delicious, and using it liberally can help to make your diet highly satisfying.
Have a question you’d like to have answered? Email me at hello@ibsgamechanger.com
More Deliciously Low FODMAP™ Tips and tools
Eat Your Way to Happiness! (Low FODMAP)
When you’re ready to start eating your way to happiness, you can find over 100 plant-forward recipes in my recipe club, perfect to expand your diet, nourish your gut biome, and support the production of your happiness brain chemicals.
If you have IBS, you’ve heard terms like “gut brain” or “second brain” before but you may not really understand what that means—and why it’s so important for those of us with IBS. Ordinarily, we talk about the gut-brain in terms of the response to food and FODMAPs. In this article, we’re focusing on the role of the gut in regulating mood. Did you know that your gut bacteria produce a whopping 95% of your serotonin (the primary “happiness neurotransmitter”) and about 50% of your dopamine (another “happiness neurotransmitter”)? In fact, your gut produces MORE neurotransmitters than your brain does!
It seems clear then, that when your gut bacteria are not happy, you are not happy either! So, let’s talk about eating your way to happy which means we will be focusing on “Psychobiotic health” a term used by researchers to refer to gut microbes that benefit mental health.
How do you promote healthy, happy, and flourishing gut bacteria? Read the full article, written by my amazing sister, Sarah Aitken, RN, MS, WHNP/FNP, NBC-HWC, to learn how to avoid going Psycho by going Psychobiotic!
When you’re ready to start eating your way to happiness, you can find over 100 plant-forward low-FODMAP recipes in my recipe club, perfect to expand your diet, nourish your gut biome, and support the production of your happiness brain chemicals.
More IBS Game Changer Tips and Tools
Bringing the experts to you - Free Virtual Speaker Series: IBS Secrets Revealed
I am honored to be a part of this digestive health summit and I have a complimentary ticket for you to attend totally free.
One of the biggest challenges when struggling with gut issues is finding answers. It should be easy, but you and I both know it’s not.
My friend and colleague, Kelly Cleveringa of Clever Body Wellness, hosted a speaker series she called IBS Secrets Revealed that brought together a group of experts from all areas of the gut health spectrum to offer all sorts of advice for improving your digestion and enhancing your life. I was honored to be a part of this digestive health summit and I’m sharing the on-demand link so you can watch the entire series, or just pick the topics that interest you most.
There were 15 expert speakers in this virtual summit talking about different areas of living with and treating IBS.
These amazing experts included…
Katherine Aitken-Young from IBS Game Changer
Heather Van Vorous from Help for IBS
DeDe Wilson from Fodmap Everyday
Helen Brooks from The Tummy Whisperer
Amy Laura from FODify It
And many more!
When you’re at the right table with the right people, you heal faster than you ever could on your own. This is the right table which is why I’m thrilled to have been included as a speaker and I want to share the content with you!
Have a question you’d like to have answered? Email me at hello@ibsgamechanger.com
Check out my latest Deliciously Low FODMAP™ recipes
Manage Your IBS Symptoms with Yoga—Poses to Calm Your Belly and Your Mind
When a recent clinical study confirmed, “Yoga may be as effective as pharmacotherapy, cognitive-behavioral therapy, exercise, and the low FODMAP diet to reduce IBS symptoms, symptoms of anxiety and depression, and stress in patients with IBS,” I was convinced yoga should be considered an important part of managing IBS.
When I eat the wrong thing, eat too much, or feel extra stressed, my IBS Symptoms flare up. And, over the holidays, I did a lot of all of those things. This year, however, instead of taking to my bed or curling up on the bathroom floor, I had an awesome new tool in my toolbox—yoga! I discovered yoga thanks to my amazing daughter and, since I started practicing yoga regularly, I have seen many benefits to my overall health and well-being—including significant benefits to my IBS symptoms in particular. When a recent clinical study confirmed, “Yoga may be as effective as pharmacotherapy, cognitive-behavioral therapy, exercise, and the low FODMAP diet to reduce IBS symptoms, symptoms of anxiety and depression, and stress in patients with IBS,” I was convinced yoga should be considered an important part of managing IBS.
There are a few yoga poses, in particular, that are calming to your gut and that’s what I’m sharing with you here. Don’t worry, you don’t have to find a yoga studio and sign up for classes right away, just follow the guidance in this article to add some yoga moves to your day and you might just find you feel the benefits—and you’re hooked!
My friend Alexandra Edwards is an amazing human being and practitioner of movement medicine and owner of Monterey Bay Contrology in Monterey, California. Ali was kind enough to sit for pictures of some of the poses that are good for your gut so you can see exactly what you’re going for. Whether you’re having IBS symptoms or not, I hope this article inspires you to give yoga a try.
Seated side twist (Parivrtta Sukhasana)
Sit down on the floor and cross your legs. Take a deep breath in and lengthen your spine and the sides of the body, then turn and put your right hand on your left knee, and steady yourself with your other hand behind you. Breathe out and gently twist while looking over your left shoulder.
Hold this pose for five slow breaths, then release and repeat on the opposite side.
Focus on drawing your navel towards your spine at the end of each exhalation.
Seated side bend (Parsva Sukhasana)
Sit down on the floor and cross your legs. Start your side stretch by taking a deep breath in and raising your left arm, then exhale and stretch the left arm over to the right, bending into a side stretch and supporting yourself with your right arm. Think of elevating on the left side of your body not collapsing on the right. Hold for five breaths. Repeat on the other side. Look up to the ceiling as shown for a greater stretch.
Cat-cow (Chakravakasana): Cow
Make your way to your hands and knees with your hands under your shoulders and your knees under your hips.
Take a deep breath in, draw your navel to the floor, look up to the ceiling, and exhale. This is the "cow” part of Cat-Cow.
Then go to the “cat” part of Cat-Cow and repeat 5-10 times.
Cat-cow (Chakravakasana): Cat
From the “cow” position, take a deep breath in as you arch your back to the ceiling like a cat stretching. Think of drawing your navel toward your spine as you do this, tuck your tailbone down, open the space between your shoulder blades, and let your head drop. Then go back to the “cow” part of Cat-Cow and repeat 5-10 times. Align the movements of Cat-Cow with your breath: in for cat and out for cow.
Sun salutation (Surya Namaskar)
Sun Salutation is a series of yoga poses performed in a sequence to create a flow of movement. Watch the video below to see the combination of movements that make up the complete sequence.
Start standing up with your toes touching and your heels slightly apart. Take a breath in and raise your arms to the ceiling, exhale, and fold forward touching your hands to the floor
Take another breath in and raise up halfway with your fingertips on the floor or lightly touching your shins. Exhale, and return to forward fold.
Bend your knees, place your hands on the floor below your shoulders, and then step your left leg back into high lunge. Next, step your right leg back so you are in a plank position. Hold this pose for a breath or two or flow right through it to the next part of the sequence.
Bend your knees and go through the following Chaturanga sequence (Chaturanga: from plank position, exhale, lower yourself down to the mat evenly as though doing a push-up, as you breathe in, straighten your arms while leaving your hips on the floor to move into upward facing dog; breath out and move into downward facing dog) hold for a breath, step your left leg forward into a lunge, then step your right leg forward to meet your hands in forward fold at the top of the mat, inhale and stand up lifting your arms toward the ceiling, bring your hands to heart center (prayer) to finish.
Do this same sequence on the opposite side, then do each side again once more. Two full sequences are a great way to stretch and massage your belly.
Locust pose (Salabhasana)
Lie on your stomach with your arms by your sides. Engage your gluteal (butt) muscles and, as you take a breath in, lift your head, upper torso, arms, and legs away from the floor. Don’t lift so high that you feel a pinch in your low back and be sure to tuck your pubic bone/lower abs in.
Exhale and release to the ground. Repeat this pose five times and try to hold each time for five breaths in and out.
Bow pose (Dhanurasana)
Lie on your stomach with your arms by your sides. Bend your knees and take hold of your ankles or feet. (If you can't reach your ankles or feet, you may use a strap or towel.) Engage your back and gluteal (butt) muscles and as you take a breath in, lift your head, upper torso, arms, and legs away from the floor. With strong legs and arms, gently pull on your ankles/feet to create the shape of a bow (like a bow and arrow).
Once you’re in this position, use your breathing to create a rocking motion to stimulate your digestive tract. Inhale to let the upper abdomen expand and exhale to contract. After five inhalations and exhalations (or sooner if you have any discomfort) release to the ground.
Knees-to-chest (Apanasana)
Lie on your back. As you take a breath in, slowly bring both knees to your chest and hug them into your body. You can grasp your wrists or your elbows, whatever is most comfortable. Try to keep your shoulders on the floor. Rock side to side if you like. Hold this position for five breaths.
Reclined spinal twist (Supta Matsyendrasana)
Lie on your back and extend your legs. Take a breath in and, as you breathe out, hug both knees into your chest. Stretch your left leg out, keeping your right leg hugged in. Place your left hand on the outside of your right knee and gently pull it over to the left. Extend your right arm straight out to the right, turn your head to the right. Relax and hold the pose for at least 10 slow breaths. (You can adjust this pose by moving both legs to one side if that’s more comfortable.)
To switch to the other side, slowly come back to center, hug both knees into your chest and repeat on the other side.
Reclining bound angle pose (Supta Baddha Konasana)
Lie down on your back. Place the soles of your feet together and allow your knees to gently fall apart. Focus on breathing from your belly, not your chest. To help with this, you can put one hand on your belly and the other hand on your chest and try to breathe so only the hand on your belly rises.
You may use blankets or pillows to support your knees and make yourself comfortable. Do slow, deep breathing and stay in this pose for five minutes or as long as you are comfortable.
Corpse pose (Savasana)
This could be the best asana of all so don’t skip it!
Lie on your back with your legs and arms extended and slightly spread out. Allow your legs to relax and turn out to the side. Close your eyes. Focus on breathing from your belly, not your chest. To help with this, you can put one hand on your belly and the other hand on your chest and try to breathe so only the hand on your belly rises. Stay in this position for five minutes or more as you relax in this pose.
Come out of this pose slowly by rolling onto your side first and resting in fetal pose (Parsva garbhasana) for a few breaths before coming up to a seated cross-legged position. Rest for a few breaths before standing.
Navigating The Holidays Without IBS Flare-ups
What you need to know about navigating the holidays without IBS flare-ups.
The holidays are fraught with opportunities to eat and drink all kinds of foods that aren’t in our normal daily diet, and to be with people or in situations we may or may not be comfortable with. That means those of us with IBS often spend much of the holidays not feeling our best or, even worse, feeling terrible. Why is that? Because we are surrounded by food, drink, people, and situations that are likely to be full of IBS triggers and we can’t (or won’t) say no because we are concerned about what others might think about us. So what do you do about that?
If you’ve managed to get your IBS under control, then you’re pretty aware of the triggers that affect you. And, when you know your triggers, you know what happens if you dive in and eat or drink things that will trigger you: You’ll have a flare-up! (If you haven’t gotten your IBS under control consider making that your New Year’s resolution and let’s talk!)
Instead of closing your eyes, accepting every invitation, and eating and drinking whatever is offered, ask yourself why you are not comfortable declining things that will make you feel sick.
Thank you to my amazing sister, Sarah Aitken, RN, MS, WHNP/FNP, NBC-HWC, for the collaboration on this post.
My friend and I had a conversation the other day, and we were talking about the feeling of pressure to “try this amazing onion dip” when everyone else was raving about it. Or garlic mushrooms, or whatever other food is being served.
I have absolutely NO problem saying "no" to food that I know will make me sick. It bothers me not in the least, not even a pang.
My friend, on the other hand, has LOTS of drama around it. She pretty much felt it was just too painful and she couldn't do it. She didn't want people to think she was “on a diet.” She didn't want to be the "party pooper." She didn't want to be "that person." She felt, by declining, the hostess would be insulted and the party would be ruined for her and everyone else.
But she has no trouble at all saying "no" to a special holiday cocktail. She is just not a big cocktail lover.
And I have drama around that one (although I'm much better than I used to be!).
So, what's the difference? Why are we absolutely fine being the "different one" in one situation, and not in another?
The difference lies in our thoughts, and it is US who are the ones being judgmental.
Her thoughts reflect her OWN judgments about herself and other people saying "no" to food, not the thoughts of those around her. It is SHE who would be thinking, "Is that woman on a diet?" "What a party pooper." "Well, she's sure a problem to invite to a party." "Oh great, we have a health nut in the crowd."
She herself is a judgmental person.
With that in mind…here’s the fix!
Stop. Being. So. Judgmental.
(And you know what that is? A slightly judgmental statement on my end – that you should be less judgmental. See how hard it is to get away from these things?)
How do you do that?
Develop self-awareness by observing your thoughts.
Learn to catch yourself in the act. Listen to your thoughts. Look for phrases such as:
That person shouldn’t do _____________[action].
If I were that person, I wouldn’t do ____________[action]; I would do _____________[alternative action] instead.
That person is so ______________ [negative adjective].
Once you learn to recognize these thoughts, ask yourself why you feel the need to judge the people in question.
Take note of what triggers your judgmental thoughts.
Judgments can be either positive or negative; in either case, you’re assuming you know the full situation and the reasons behind someone’s behavior.
Next time you catch yourself making a judgment about others, turn it into an opportunity for introspection.
Why do you think the other person’s actions pushed your buttons?
How can you work on improving those beliefs or insecurities? How is what the other person is doing/saying any of your business?
For example, you might be more judgmental when you’re around certain people, in certain environments, or when you’re feeling a certain way. Learning to recognize these triggers is an important step toward becoming less judgmental.
Practice empathy.
In most cases, if someone is doing something you are judging harshly, you won’t know their motivation unless you ask them about it. If you can ask politely and with a genuine sense of curiosity, go ahead and ask! If you can't ask with that mindset, then practice some empathy and open your mind to various possible explanations for their behavior and their choices. Give people the benefit of the doubt.
Be accepting.
Once you’ve tried understanding the other person, accept them for who they are. It’s really hard to change someone else. In fact, succeeding is highly unlikely. Only they can change themselves, as only you can change yourself.
You don’t have to be their best friend or even like them, but see if it is possible to avoid judging them or letting negative thoughts fester in your mind.
Show yourself compassion.
Your judgment of others reflects your judgment about yourself and therefore your actions and reactions. Once you dial down your judgmental mind, you may find it gets easier to say “no thank you” to food, drink, stressful situations, or even certain people, that you know will trigger a flare-up. You might just discover a wonderful sense of freedom when you give yourself permission to politely decline—without judgment or concern. No need to apologize. No need to make a big deal.
And remember, nobody is perfect, and you’ll probably stumble quite a few times in your quest to be less judgmental. Forgive yourself and keep trying. And have a wonderful holiday season no matter what.
Want to learn more about how to get your IBS under control?
What You Need to Know About GERD and Low FODMAP
What you need to know about GERD and the Low FODMAP diet
Those of us who have IBS often have companion problems related to our digestion that can cause us unnecessary pain and suffering. One of those potential companion problems is GERD or (Gastroesophageal Reflux Disease). There’s a lot of misinformation about GERD out there and there’s even more information that is correct, but very difficult to understand. With that in mind, I am sharing an excellent guest post written by an expert (who just happens to be my amazing sister), Sarah Aitken, RN, MS, WHNP/FNP, and featured in her own Game Changer program.
GERD can be the cause of heartburn, difficulty swallowing, burping a sour taste, excessive coughing or throat clearing, and more. Thankfully, many of the foods we can eat freely even while on a low FODMAP diet, actually help prevent GERD. And, lots of the foods we may already restrict on a low FODMAP diet are the ones that can make GERD worse. So, if you’re truly following a low FODMAP diet, you may already have cured yourself of GERD symptoms. But, if you’re having symptoms even while you’re following a low FODMAP diet, then this article just might give you the additional information you need to improve your symptoms.
Want to learn more about how to follow a low FODMAP diet? You can get learn more right here.
What You Need to Know About Bread and IBS
There’s more to bread than meets the eye, especially for those of us with IBS!
When you have IBS you are often advised to become “gluten-free” and bread is the first thing to go from your diet. I love a good whole grain bread and I’m here to tell you (or remind you if you already know) that a low FODMAP diet is not intended to be gluten free! As discussed in my previous article, Gluten vs Fructans Who’s the Culprit the FODMAP trigger in bread is the Fructan, not the gluten. That’s not to say some of us with IBS aren’t also sensitive to gluten itself—but that’s a separate issue.
There’s more to bread than meets the eye, especially for those of us with IBS, and this article (written by my amazing sister, Sarah Aitken, RN, MS, WHNP/FNP for her Game Changer Program) is going to help you understand how and why your body responds differently to different types of bread so you can steer your eating towards the best bread choices for you.
Did you know, when you eat a piece of regular white bread, or regular whole wheat bread, you are converting the starches in that bread immediately to sugar (glucose)? And, when you do that, your blood sugar rises higher and faster than if you just ate a piece of candy?! What happens next? You get a drop in your blood sugar which leads to feeling tired and low energy. Then, you might reach for a cup of caffeinated coffee—which in turn triggers your gut. It’s a classic combination that leads IBS sufferers into a self-induced flare-up or an afternoon of exhaustion.
But, lucky for us, there are amazing breads that have a much less powerful effect on our blood sugar and on our gut!
What you need to know about FODMAP Stacking
What you need to know about FODMAP Stacking
When you’re on a low FODMAP diet and trying to avoid triggering your IBS symptoms, you get very familiar with what foods contain what FODMAPs and what is considered a “safe” serving size. But what if you are sticking to safe servings sizes and you’re still having symptoms? This may be the result of FODMAP stacking.
What is FODMAP stacking? When you have multiple “safe” servings of different foods containing the same FODMAP, or multiple servings of foods containing different FODMAPs and the combined effect causes you distress, this is what we refer to as FODMAP stacking.
Important note: There is no need to worry about FODMAP stacking if your symptoms are well controlled. If, however, you’re still having symptoms while following a low FODMAP diet, then FODMAP stacking may be a contributing factor. Read on.
This article is adapted from this post by Monash University
Are FODMAP amounts cumulative?
The short answer is, yes. In one sitting, the total amount of FODMAPs consumed (be it from fructose, fructans, lactose, GOS, or polyols) influences whether the meal is tolerated or whether symptoms are induced.
The Monash University FODMAP diet app uses a traffic light system to indicate the rating of each FODMAP in individual foods (fructose, sorbitol, mannitol, lactose, fructans, and GOS), and the overall FODMAP rating (low (green), medium (yellow), high (red)) of foods at different serving sizes. But we know that people don’t just eat individual foods, they eat mixed meals including multiple different foods. For this reason, the Monash recommendations for low FODMAP serving sizes were set conservatively, allowing people to include more than one green light serving of food per sitting.
Everyone’s threshold level of FODMAP tolerance is different. While FODMAP stacking will be relevant to some people who may find they experience IBS symptoms when multiple green light servings are eaten in one sitting, for many, the conservative FODMAP serving sizes set by Monash means they will achieve good symptom control even when consuming a varied diet that includes numerous green light servings at each sitting.
Does FODMAP stacking relate to the foods eaten over a whole day or just in one meal?
As a general rule, the concept of stacking relates to a single sitting or meal. This of course assumes that meals are spaced out over the day, with at least 2-3 hours between each meal or snack. This allows food to be digested between meals and slows the rate at which the gut is exposed to the FODMAPs. If you find you are constantly snacking and experiencing IBS symptoms, then spacing out your meals may help.
Do I need to track what FODMAPs I eat to avoid stacking?
First of all, if your symptoms are well controlled and you haven’t been thinking about FODMAP stacking, then don’t start worrying about it now! It doesn’t apply to you and the low FODMAP diet is working for you just fine.
You only need to consider FODMAP stacking if you notice that a low FODMAP diet has improved most of your symptoms, but not all of them.
For some people, it will be factors other than FODMAPs that are affecting their IBS symptoms such as stress, hydration, exercise, or anxiety. For others, it might be a higher sensitivity to FODMAPs and thus a need to consider FODMAP stacking as a possible trigger. If you think this applies to you, keeping a food and symptom diary is the best way to work out what your individual IBS triggers are, and whether FODMAP stacking is an issue for you.
Key Tips and Takeaways to Avoid Consequences:
Space out your meals. Leave at least 2-3 hours between eating or drinking anything other than black coffee or water (that includes meals, snacks, and beverages) to avoid potential stacking effects.
Avoid snacking. If you find you are getting hungry between meals (and I’m referring to actual hunger, not boredom, stress, or emotional eating) make sure your meals include enough protein, fat, and fiber to fill you up and keep you satisfied until the next meal.
If you must have a snack, choose a snack that is low in FODMAPs and high in food value such as a protein food (eggs/meat/fish/nuts/nut butter), a complex carbohydrate (whole grain such as whole grain sourdough bread or brown rice), or plants such as carrots or cucumbers.
What does that look like? How about a hard-boiled egg and some black olives? Or a brown rice cake with a slice or two of turkey and some sliced cucumbers on it? Or, a slice of whole grain sourdough with peanut butter on it. Or, a small handful of mixed nuts such as macadamia, pecans, almonds, etc. More snack ideas can be found on my blog here.
More Deliciously Low FODMAP™ tips & tools
Blood Sugar Hacks for Optimal Energy, Sleep, Mental Clarity, and More
Even if you have no blood sugar “problems,” eating for optimal blood sugar control will very likely make you feel better, maybe even in some unexpected ways!
Article by Sarah Aitken, RN, MS, FNP/WHNP, Game Changer
Sharing this excellent article, written by my amazing sister, because it has great advice for ALL of us. Our bodies crave homeostasis (staying at a steady state) and our diet tends to send us on a daily roller coaster. In this article, you’ll learn some excellent strategies to stay off that roller coaster and give your body and mind some peace.
There are many reasons why you feel most optimal if your blood sugar is well controlled. Blood sugar swings are largely responsible for a multitude of symptoms, including that “hangry” feeling, hypoglycemia (assuming it is not caused by hypoglycemic medications), fatigue, fuzzy headedness, excessive hunger, cravings for sugar and fat, body inflammation, brain fog, and weight gain, among others.
Even if you have no blood sugar “problems,” eating for optimal blood sugar control will very likely make you feel better, maybe even in some unexpected ways!
Better sleep, longer attention span, gentler menopausal or PMS symptoms, better body temperature control – all those things are possible with optimal blood sugar levels.
Who doesn't want all that??