Deliciously Low FODMAP
Inspire yourself with hundreds of delicious low FODMAP recipes, tips, and tools, and enjoy the abundance that is yours even when you have IBS.
Use the buttons and filters to find something specific or browse the complete collection for inspiration.
Discover a treasure trove of recipes with my FREE recipe club! Get new ideas delivered straight to your inbox every week.
Deliciously Low FODMAP is a trademark of IBS Game Changer, LLC
Filter to find Recipes and Tools
More Filtering Options
- All 794
- Appetizer 55
- BBQ 49
- Bowl 32
- Breakfast 69
- Cocktails 13
- Collection 1 58
- Collection 10 27
- Collection 11 30
- Collection 12 27
- Collection 13 31
- Collection 14 29
- Collection 15 31
- Collection 16 34
- Collection 17 31
- Collection 18 33
- Collection 19 36
- Collection 2 32
- Collection 20 33
- Collection 21 33
- Collection 22 40
- Collection 23 62
- Collection 24 15
- Collection 3 28
- Collection 4 29
- Collection 5 30
- Collection 6 32
- Collection 7 31
- Collection 8 31
- Collection 9 32
- Condiments 6
- Crock Pot 4
- Dessert 117
- Diabetes Game Changer Exception Protocol Contains Alcohol 11
- Diabetes Game Changer Exception Protocol Contains Flour 113
- Diabetes Game Changer Exception Protocol Contains Flour AND Sugar 79
- Diabetes Game Changer Exception Protocol Contains Sugar 52
- Diabetes Game Changer First Four Weeks 404
- Dinner 362
- Drink 8
- Easter 1
- Free Guide 17
- Gluten-free 653
- Gut Microbiome 2
- Guthealth 3
- Holidays 73
- IBS Triggers 4
- Keto Friendly 163
- Lactose-Free 181
- Low Carb 8
Mastering Mindful Eating: 13 Essential Strategies to Detox from Mindless Munching
After the holidays or any time you want to improve your relationship with food, use these techniques to master mindful eating and regain control of your health.
For better or for worse, the holidays are often focused on food. And not just healthy, nourishing food, but food that may be extra rich, extra sugary, and full of FODMAP Triggers. So how do you get back to a mindful mindset when it comes to eating? Detoxing from mindless eating involves building (or rebuilding) mindful eating habits and breaking free from automatic, unconscious consumption. In this blog post, I am sharing some steps to help you regain control and foster a more mindful relationship with food.
You can start by creating a focus on what your body needs, not what your primitive brain wants. This will help you make decisions and prioritize those decisions that support your focus on health. For me, that focus is captured in this variation on Michael Pollan’s philosophy on food: Eat real food. Mostly plants. Prepare it yourself.
Read on for some specific things you can do to help yourself reset after the holidays.
Raise Awareness:
Start by acknowledging and recognizing your mindless eating habits. Be aware of situations, emotions, or triggers that lead to unconscious eating.
Be Mindful:
Engage your senses when eating. Sit down and pay attention to the food on your plate. Notice the colors, textures, and flavors of your food. Chew slowly. Savor each bite. This helps you appreciate your food and recognize the signals your body sends when you have had enough.
Create a Distraction-Free Zone:
Designate specific eating areas and times. Avoid eating in front of the TV, or computer, or while scrolling through your phone. Minimize distractions so you can focus on your meal.
Control Your Portion Sizes:
Eat your meals on a plate or in a bowl to maintain a clear sense of how much you’re eating and encourage appropriate portion sizes. Don’t eat out of the container, bag, or carton. This can help prevent overeating.
Meal Planning:
Plan your meals in advance. Having a structured eating schedule reduces the likelihood of impulsive, mindless eating.
Stay Well-Hydrated:
Stay hydrated throughout the day. Sometimes, feelings of hunger are actually signals of dehydration. Start your day with a big glass of water (this can also help regulate your bowel movements). Drink water before reaching for a snack, then wait 15 minutes to be sure you're truly hungry before eating.
Listen to Hunger Cues:
Pay attention to your body's hunger and fullness signals. Eat when you're hungry and stop when you're satisfied, rather than relying on external cues or emotional triggers. Don’t eat so fast that you zoom right past your body’s ability to let you know it’s full! Slow down, chew your food, and put your fork down between bites.
Mindful About Snacking:
If you can break the habit of snacking altogether, that’s a great way to minimize mindless eating. But, if you want to keep snacks in your diet, choose them thoughtfully. Opt for real food here too, and something with protein, fiber, and fat that will be filling and satisfying (a handful of nuts, a few of my Amazing Seed Crackers with cheese or Nutzo Nut & Seed Butter, or some chopped vegetables and lactose-free cottage cheese or Nutzo Nut & Seed Butter are great choices). Be conscious of portion sizes. Sit down and savor your snack rather than eating it on the go.
Emotional Awareness:
Identify emotional triggers for mindless eating. When you feel stressed, bored, or anxious, find alternative ways to cope, such as taking a short walk, practicing deep breathing, or engaging in a hobby. Work on just feeling your emotions instead of letting them drive you to the kitchen to drown them in a bag of chips or a box of cookies. If you give them time, these feelings usually pass within a few minutes, and you can avoid the need to buffer them with food.
Keep a Food Journal:
Track your meals and snacks in a journal or phone app. This helps you become more aware of what, when, and how. much you eat, making it easier to identify patterns of mindless eating. It’s a great way to be “onto yourself” about portions and portion sizes too.
Mindful Grocery Shopping:
Plan your meals and related grocery shopping list ahead of time and stick to it. Avoid shopping when hungry, as this can lead to impulse purchases of unplanned and less nutritious foods.
“Safe” Refrigerator and Pantry Shelves:
Clear out your fridge and pantry of the foods that you tend to eat mindlessly. Often that means the highly processed salty, sugary, or fatty foods that come in boxes and bags. If you live with others and the refrigerator and pantry are shared, then establish certain shelves that are just for you and that contain only the foods you want to be eating. Then you can focus only on those shelves when you’re hungry or preparing a meal. Avoiding temptations is a huge step in the direction of preventing mindless eating in the first place!
Seek Support:
Share your goals with friends, family, or a support group. Having a supportive network can provide encouragement and accountability on your journey toward more mindful eating.
Remember, developing mindful eating habits takes time and patience. Be kind to yourself throughout the process, celebrate small victories, and gradually integrate these practices into your daily life for a sustainable and positive transformation. The more you practice these techniques, the less you overload your body and the better you feel. It’s something to look forward to!
Need help on your journey? Make an appointment and let’s talk!
Have a question you’d like to have answered? Email me at hello@ibsgamechanger.com
Link note: This post may contain affiliate links for you to easily purchase items that are linked. I may earn a small commission from qualifying purchases but none of this costs you a thing so feel free to use the links! In addition, for some items, I have provided a special discount code for IBS Game Changers so be sure to use the code when you purchase an item to get the discount that has been arranged just for you.
More Deliciously Low FODMAP™ Tips and Tools
How to Identify FODMAP-Free Foods Like a Pro
Tips for identifying FODMAP-free foods
Navigating the low FODMAP diet can feel overwhelming, but knowing which foods are FODMAP-free makes meal planning so much easier! If you’re using the Monash FODMAP App, spotting FODMAP-free foods isn’t always obvious at first glance.
Here’s the trick:
Click on a food in the app (e.g., chicken)
Confirm the app ONLY shows a "green” serving size of that food (if there are any yellow or red traffic light colors, move on because that food DOES contain some FODMAPs)
Scroll down past the one section of green traffic lights
Look for the phrase “Please note that the ‘green’ traffic light rating system allows you to eat multiple serves of ‘green’ foods per meal.”
If you see this statement, combined with ONLY a green light serving size, you’re in the clear! These foods are officially FODMAP-free, meaning you can enjoy multiple servings in one sitting. Note: As with any food, too much of one thing can be hard for your system to digest—so continue to eat a variety of foods with every meal and snack.
Let’s Talk Protein!
Good news—all meats are naturally FODMAP-free! This makes them an excellent foundation for your meals (keeping in mind, marinades and seasonings may contain FODMAPs so be aware of those). Here are some high-protein, FODMAP-free options:
✅ Chicken
✅ Beef
✅ Pork
✅ Lamb
✅ Fish
✅ Seafood
✅ Eggs
What About Veggies?
Adding FODMAP-free vegetables to your plate ensures you’re getting plenty of fiber without triggering symptoms. Here are some excellent go-to options:
🥔 Potato
🥬 Arugula (AKA Rocket)
🥕 Carrot
🥒 Cucumber
🎃 Patty pan squash (AKA button squash)
🥬 Lettuce, red coral (red leaf)
🥄 Pickled beetroot
🌰 Parsnip
🍃 Rhubarb
Are There Any FODMAP-Free Fruits?
Yes! But keep in mind that even FODMAP-free fruits should be limited to one serving per sitting (1 cup chopped, 1 medium piece, or 2 small pieces). Some great choices include:
🍌 Firm, banana (no spots)
🍍 Yellow papaya
🍊 Mandarin orange
🍊 Navel orange
🍈 Dragon fruit
🥭 Guava
Other Handy FODMAP-Free Foods
Want to add more variety? Here are some versatile FODMAP-free staples:
🧄 Chives
🫚 Ginger
🥛 Plain lactose-free yogurt
🥛 Lactose-free milk
🍚 Rice
🫒 Olives, olive oil, avocado oil
5 Easy FODMAP-Free Meal Ideas
Ready to put it all together? Here are five simple, delicious meal ideas made entirely with FODMAP-free ingredients:
🥩 Meat & Roasted Veggies – Roasted root veggies (potato & carrot) tossed with extra virgin olive oil, salt, and, pepper.
🐟 Salmon & Salad – Baked potato with a salad of arugula and cucumber tossed with a simple oil and vinegar dressing.
🍗 Chicken Stir-Fry – Sautéed chives, ginger, carrot & parsnip served over rice.
🥚 Veggie Frittata – Eggs, potato, patty pan squash & chives topped with grated cheese.
🍨 Tropical Yogurt Bowl – Plain lactose-free yogurt with diced yellow papaya & dragon fruit.
Final Tips
All FODMAPs are carbohydrates (although not all carbohydrates are FODMAPs). So, if a food contains no carbohydrates, it also contains no FODMAPs.
Foods and portion sizes change as research evolves. Always check the Monash FODMAP App for updates before digging in!
Now, eat and enjoy every bite, because you can! 🎉
Stop letting discouragement derail your health: 8 Tips that work
In this blog post I’m sharing 8 strategies to overcome the feelings of discouragement and fear that may be standing in the way of your success.
Okay, friends, let's talk guts—both the kind churning with IBS and the kind it takes to face a challenge. If you're a regular to my blog, you know my amazing sister, Sarah Aitken (RN, MS, WHNP/FNP, MHP, NBC-HWC—yes, she's that impressive), runs a fantastic program focused on diabetes and pre-diabetes. Now, you might be thinking, "Diabetes? What's that got to do with my perpetually grumpy gut?" Well, Sarah's insights often overlap beautifully with the IBS world, and her latest article about finding courage in the face of feeling discouraged and afraid? Pure gold. Seriously, give it a read. And if you want more wisdom delivered straight to your inbox (because who doesn't love a little Monday Motivation?), sign up for her newsletter right here. Trust me, your inner (and outer) self will thank you. Want to listen instead of read? Released every Monday, Sarah’s podcast, available on Apple Podcasts and Spotify is delightfully educational and entertaining.
Republished with permission of Sarah Aitken
Discouraged. It’s an emotion I’ve been experiencing while dealing with a serious website problem for the last week.
I took a moment to really look at that word. It means lacking courage. Feeling scared.
Embarking on radical lifestyle change (for most people, eating in a way to reverse insulin resistance IS a radical change) requires courage. Will it work for me? Will I be able to stick to it? Can I design an eating plan that feels sustainable so that I can remain on it forever? I had a setback. Will I ever get back on track?
Taking a leap of faith requires courage. Getting back on track requires courage. Sticking to something in the face of adversity requires courage.
Courage means you are not allowing circumstances to get the best of you. It is making the right decisions in the face of fear. It is getting back on that horse and trying it again. It is taking risks and dealing with uncertainty. It is making “bravery” a habit.
Being courageous doesn’t mean you are not afraid. It means you are doing something even though it scares you to do it.
Here's some great news: courage can be learned and cultivated!
Here are 8 ways to overcome the feeling of “discouraged” when fear has you stuck:
Acknowledge that when you feel discouraged, it is not because you can’t do something, it’s because you are letting fear stop you from trying again. Face the feeling of fear. Sweeping it under the rug gives it power. Courage is not about eliminating fear, it’s about moving forward in spite of fear being present.
Confront the feeling and become curious about it. What is it about the present situation that is scaring you? What would happen if you felt more courageous about it? Could it be that you are protecting your ego from experiencing failure? The reality is, continuing to try in spite of setbacks and failures makes you stronger and more resilient.
Get comfortable with being uncomfortable. Dale Carnegie once said, “Do the thing you fear to do and keep on doing it...that is the quickest and surest way ever yet discovered to conquer fear.”
Make doing brave things a habit. Consciously strengthen your courage like a muscle by practicing it. In her book Fear Is Not An Option author Monica Berg recommends making a list of things that you would do if you weren’t afraid. If you made a list, what would it look like? Could you start doing some of those things now?
Fear is often a pretend worry about something that MIGHT happen, but which is not actually happening right now. What are some other outcomes that are just as likely? Give equal airtime to alternate thoughts regarding the future and stay grounded in what is happening right now.
Embrace failure! Success is much less about succeeding perfectly and much more about tolerating the failures along the way. Get curious about failure – see what you can learn from it. Build your resilience muscle!
Don’t aim for perfection. Approach the problem with a beginner’s mind. Let go of expectations of how it’s going to go and get curious about it. Stop worrying about the outcome.
See fear as an opportunity instead of a roadblock. Fear can even be a handy guide, showing you the areas of your life that need some work.
For me, just writing this article has helped me feel less discouraged about my website problem. I feel a little more courageous, and I’m glad that one silver lining is that once the problem is fixed, I will be all the more able to overcome the next challenge with less fear.
More Deliciously Low FODMAP™ Tips and Tools
I’ve got IBS. What do I do now?
Take Control of Your IBS: Your Journey Starts Here
Take Control of Your IBS: Your Journey Starts Here
Living with IBS can be frustrating and confusing. But you're not alone, and you don't have to suffer. In this post, I'll share practical tips and insights to help you navigate your IBS journey.
Discover how to:
Uncover Your Triggers: Learn the power of journaling to identify your unique sensitivities.
Build a Strong Foundation: Prioritize lifestyle factors like sleep, stress, and movement for optimal gut health.
Understand the Science: Gain knowledge about the mechanisms behind IBS and FODMAPs so you can make informed decisions.
Read on to learn how to take control of your IBS and improve your quality of life.
If I’m not coaching, you’ll find me in my kitchen cooking up a new recipe for my Deliciously Low FODMAP recipe club!
IBS: Your Next Steps
So, you've been diagnosed with IBS. While it might feel overwhelming, there's a lot you can do to manage your symptoms and improve your quality of life.
As a healthcare professional with firsthand experience, I've found that three key steps can significantly impact your journey:
1. Journal Your Journey
Before diving into dietary changes, start a food journal. Track your meals, drinks, symptoms, stress levels, and other lifestyle factors. This baseline information will help you identify potential triggers and measure the impact of your interventions.
2. Build a Strong Foundation
While FODMAPs are often culprits in IBS, they're not the only factors. Lifestyle habits like sleep, stress management, and physical activity play a crucial role. Prioritize these areas to enhance your overall well-being and improve your body's tolerance to FODMAPs and other triggers.
3. Understand the Why
Knowledge is power. Before making dietary changes, take the time to understand the underlying mechanisms. Why do certain foods trigger symptoms? How do FODMAPs impact your gut? By grasping the "why," you can make informed decisions, tailor your approach, and effectively monitor progress.
Ready to Take Control?
If you're frustrated with IBS symptoms and eager to regain control of your health, consider a comprehensive approach that addresses both diet and lifestyle. By following these steps and seeking personalized guidance, you can embark on a journey towards a healthier, happier you.
More Tips and Tools and Free Resources
Embracing the abundance of what you CAN eat without consequences is a Game Changer
Tired of feeling restricted by food limitations?
Tired of feeling restricted by food limitations? Break free from the monotony and nourish your body and gut. Explore the vast array of foods you can enjoy with the Monash FODMAP app and my recipe club. It's time to embrace a diverse and delicious diet!
Sometimes when we have issues with food, we get stuck on thinking about all the things we can't eat. And, we end up "painting ourselves into a corner" and eating the same thing over and over again. This is monotonous and boring. And, it means you suffer, your gut biome suffers, and it can lead to "cheats" that cause major flare-ups. How can you change that cycle? Embrace the abundance of foods you CAN eat! Use the Monash app on your phone to explore foods you haven't considered. Dive into my recipe club and be a little adventurous! Make sure you have plenty of variety in every meal and snack—even if it’s not a large quantity of any one thing.
Discover new recipes in my FREE recipe club.
To streamline your search through hundreds of existing recipes, I'm moving the release of my new weekly creations to the Recipe Club on Patreon. In the club, you’ll get access to a treasure trove of low-FODMAP goodness, complete with collections and filters to use as your virtual cookbook!
Here's what awaits you in the club:
Exclusive weekly recipes: Be the first to try my latest delicious low-FODMAP creations!
Simple & Easy: My recipes continue to focus on readily available ingredients and effortless preparation, perfect for family-friendly meals (no more separate low-FODMAP meal prep!).
Hundreds of existing recipes: Gain access to my entire library of low-FODMAP recipes, all conveniently organized.
You can join for free or sign up for only $5/month. Your support fuels my passion for creating new, delicious, and easy-to-make low-FODMAP recipes just for you.
Let's go on this delicious low-FODMAP journey together.
Deep Tissue Massage for IBS Management
In this blog post, I explore some of the ways deep tissue massage can support IBS symptom management, giving you one more tool in your toolbox to find a holistic path to comfort and well-being.
Living with IBS can be challenging, with symptoms like bloating, cramping, and discomfort disrupting daily life. While dietary adjustments and lifestyle changes are common, and very effective, approaches to managing IBS, many are turning to alternative therapies for relief. One such method gaining popularity is deep tissue massage, which is known for its ability to reduce stress and improve circulation. This therapeutic practice not only helps relax tense muscles but may also alleviate some of the digestive discomfort associated with IBS. In this blog post, I explore some of the ways deep tissue massage can support IBS symptom management, giving you one more tool in your toolbox to find a holistic path to comfort and well-being.
Benefits of Deep Tissue Massage
Stress Reduction: Stress is a known trigger for IBS symptoms. Deep tissue massage can help reduce stress by promoting relaxation and lowering cortisol levels, which may help alleviate IBS symptoms such as abdominal pain, bloating, and discomfort.
Muscle Tension Relief: People with IBS often experience tension and tightness in the muscles of the abdomen and lower back due to chronic discomfort. Deep tissue massage can target these areas to release tension, improve circulation, and promote better mobility, potentially reducing the severity of IBS symptoms.
Improved Digestive Function: While direct evidence is limited, some individuals may find that deep tissue massage helps improve overall digestive function by stimulating the parasympathetic nervous system, which controls rest and digestion. This can lead to better digestion and potentially reduce symptoms such as constipation or diarrhea.
Pain Management: Deep tissue massage can help manage pain associated with IBS, including abdominal discomfort, cramping, and lower back pain. By targeting trigger points and releasing tension in the muscles, massage therapy can provide temporary relief from these symptoms.
Enhanced Mood and Well-being: Living with a chronic condition like IBS can take a toll on mental health and overall well-being. Deep tissue massage can promote the release of endorphins, which are natural mood elevators, leading to feelings of relaxation, contentment, and improved quality of life.
It's essential to consult with a qualified massage therapist who has experience working with clients with gastrointestinal conditions like IBS. Additionally, while massage therapy can provide symptomatic relief, it's important to combine it with other strategies such as dietary modifications, stress management techniques, personalized coaching, and medical treatment as needed for comprehensive management of IBS symptoms.
Have a question you’d like to have answered? Email me at hello@ibsgamechanger.com.
More Deliciously Low FODMAP™ Tips and Tools
Now on YouTube: The Diabetes IBS Connection with Katherine Aitken Young and Sarah Aitken
One of the biggest challenges when struggling with gut issues is getting answers to your many questions about cause and treatment. With this in mind, we in the content creator space, work hard to bring you specific and actionable information to help answer your questions.
In case you want to watch (AND listen to) our podcast with Dr. Tony Hampton, it is now on YouTube!
One of the biggest challenges when struggling with gut issues is getting answers to your many questions about cause and treatment. With this in mind, we in the content creator space, work hard to bring you specific and actionable information to help answer your questions.
On this episode of Dr. Tony Hampton’s podcast, Protecting your NEST, my sister Sarah Aitken, an expert in Diabetes and Insulin Resistance, and I discuss the overlapping causes of, and treatments for, Irritable Bowel Syndrome and insulin resistance. While they are distinct disorders, there are several overlapping factors that contribute to both. Tune into this podcast to learn more.
Overlapping Factors
Certain dietary factors and lifestyle habits can contribute to both IBS and insulin resistance. These include:
Processed foods: Consumption of highly processed and high-sugar foods can lead to inflammation and weight gain, both of which are linked to both IBS and insulin resistance.
Inflammation: Both IBS and insulin resistance are associated with chronic inflammation. In IBS, inflammation can lead to heightened sensitivity in the gut, causing symptoms like abdominal pain, bloating, and changes in bowel habits. In insulin resistance, inflammation can impair the body's ability to effectively use insulin, leading to elevated blood sugar levels.
Gut Microbiome: The gut microbiome, the community of bacteria living in the digestive tract, plays a crucial role in both conditions. Imbalances in the gut microbiome (dysbiosis) have been linked to both IBS and insulin resistance.
Stress: Chronic stress can exacerbate both IBS and insulin resistance.
Genetics: Genetic factors may also play a role in both conditions, increasing susceptibility.
Treatment Considerations
While the exact causes of IBS and insulin resistance are complex and not fully understood, addressing the overlapping factors can be very helpful in managing both conditions. Treatment strategies often include:
Dietary changes: Adopting a healthy, balanced diet that emphasizes whole foods, fiber, and lean protein can help improve gut health and insulin sensitivity.
Lifestyle modifications: Regular exercise, stress management techniques (like meditation or yoga), and adequate sleep can support overall health and well-being.
It's important to consult with a healthcare professional for a personalized diagnosis and treatment plan. If you are experiencing symptoms of IBS or insulin resistance, they can help you determine the best approach for managing your condition.
About Dr. Hampton’s Protecting Your NEST:
Protecting Your NEST is hosted by Dr. Tony Hampton a board certified Family Medicine and Obesity Medicine physician with a focus on helping listeners reverse the root cause of disease. The NEST and ROPE acronyms provide the foundational elements that represent the root cause of chronic disease if not mastered:
N: Nutrition (what and when you eat)
E: Exercise
S: Less stress/more sleep
T: How you Think/less Trauma
R: Relationships
O: Organism (avoiding the bad/adding the good)
P: Pollutants
E: Emotions/Life Experiences
Find Dr. Hampton’s podcast anywhere you get your podcasts. Many episodes are also available on Dr. Hampton’s YouTube channel as well.
References:
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome
International Foundation for Functional Gastrointestinal Disorders (IFFGD):
https://iffgd.org/gi-disorders/lower-gi-disorders/irritable-bowel-syndrome/
American Diabetes Association: https://diabetes.org/
Have a question you’d like to have answered? Email me at hello@ibsgamechanger.com
Check out my latest Low FODMAP and Low Starch recipes
Celebrating Four Years of IBS Game Changer: Empowering People to Live Symptom-Free
Since launching IBS Game Changer, I’ve been on a mission to support individuals living with Irritable Bowel Syndrome (IBS) by providing expert coaching, delicious recipes, and essential tips for symptom management.
I’m thrilled to be celebrating four years of helping people take control of their digestive health and improve their quality of life. Since launching IBS Game Changer, I’ve been on a mission to support individuals living with Irritable Bowel Syndrome (IBS) by providing expert coaching, delicious recipes, and essential tips for symptom management. What began as a passion for making a difference has grown into a thriving community where people can find the tools they need to feel empowered, navigate their condition with confidence, and enjoy food without fear.
Over the last four years, I’ve had the pleasure of guiding countless individuals through the complexities of IBS, offering easy-to-follow recipes, valuable advice on managing flare-ups, and a wealth of practical tools to ease the daily challenges that come with this condition. My approach goes beyond just symptom relief — I focus on helping people create sustainable lifestyle changes that lead to long-term comfort and freedom from the constraints of IBS.
To mark this milestone, I want to extend a heartfelt thank you to my clients, supporters, and followers. Whether you’ve been with me from the start or just discovered IBS Game Changer, your journey towards better health is what inspires me every day. As I look ahead, I’m excited to continue growing my offerings, expanding my recipe collection, and finding innovative ways to make IBS symptom management easier and more enjoyable.
I invite you to join me in celebrating this milestone by exploring my latest content, joining my recipe club, signing up for personalized coaching, or simply reaching out to share your own story. Here’s to four incredible years of progress, and to many more years of helping people live symptom-free, happy, and healthy lives!
Have a question you’d like to have answered? Email me at hello@ibsgamechanger.com
My latest Deliciously Low FODMAP™ recipes, tips, and tools
Podcast: The Diabetes IBS Connection with Katherine Aitken Young and Sarah Aitken
One of the biggest challenges when struggling with gut issues is getting answers to your many questions about cause and treatment. With this in mind, we in the content creator space, work hard to bring you specific and actionable information to help answer your questions.
One of the biggest challenges when struggling with gut issues is getting answers to your many questions about cause and treatment. With this in mind, we in the content creator space, work hard to bring you specific and actionable information to help answer your questions.
On this episode of Dr. Tony Hampton’s podcast, Protecting your NEST, my sister Sarah Aitken, an expert in Diabetes and Insulin Resistance, and I discuss the overlapping causes of, and treatments for, Irritable Bowel Syndrome and insulin resistance. While they are distinct disorders, there are several overlapping factors that contribute to both. Tune into this podcast to learn more.
Overlapping Factors
Certain dietary factors and lifestyle habits can contribute to both IBS and insulin resistance. These include:
Processed foods: Consumption of highly processed and high-sugar foods can lead to inflammation and weight gain, both of which are linked to both IBS and insulin resistance.
Inflammation: Both IBS and insulin resistance are associated with chronic inflammation. In IBS, inflammation can lead to heightened sensitivity in the gut, causing symptoms like abdominal pain, bloating, and changes in bowel habits. In insulin resistance, inflammation can impair the body's ability to effectively use insulin, leading to elevated blood sugar levels.
Gut Microbiome: The gut microbiome, the community of bacteria living in the digestive tract, plays a crucial role in both conditions. Imbalances in the gut microbiome (dysbiosis) have been linked to both IBS and insulin resistance.
Stress: Chronic stress can exacerbate both IBS and insulin resistance.
Genetics: Genetic factors may also play a role in both conditions, increasing susceptibility.
Treatment Considerations
While the exact causes of IBS and insulin resistance are complex and not fully understood, addressing the overlapping factors can be very helpful in managing both conditions. Treatment strategies often include:
Dietary changes: Adopting a healthy, balanced diet that emphasizes whole foods, fiber, and lean protein can help improve gut health and insulin sensitivity.
Lifestyle modifications: Regular exercise, stress management techniques (like meditation or yoga), and adequate sleep can support overall health and well-being.
It's important to consult with a healthcare professional for a personalized diagnosis and treatment plan. If you are experiencing symptoms of IBS or insulin resistance, they can help you determine the best approach for managing your condition.
About Dr. Hampton’s Protecting Your NEST:
Protecting Your NEST is hosted by Dr. Tony Hampton a board certified Family Medicine and Obesity Medicine physician with a focus on helping listeners reverse the root cause of disease. The NEST and ROPE acronyms provide the foundational elements that represent the root cause of chronic disease if not mastered:
N: Nutrition (what and when you eat)
E: Exercise
S: Less stress/more sleep
T: How you Think/less Trauma
R: Relationships
O: Organism (avoiding the bad/adding the good)
P: Pollutants
E: Emotions/Life Experiences
Find Dr. Hampton’s podcast anywhere you get your podcasts. Many episodes are also available on Dr. Hampton’s YouTube channel as well.
References:
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome
International Foundation for Functional Gastrointestinal Disorders (IFFGD):
https://iffgd.org/gi-disorders/lower-gi-disorders/irritable-bowel-syndrome/
American Diabetes Association: https://diabetes.org/
Have a question you’d like to have answered? Email me at hello@ibsgamechanger.com
Check out my latest Low FODMAP and Low Starch recipes
Good News About Avocado and FODMAPs
Monash University recently re-tested avocados for FODMAP content and they made an interesting discovery
I don’t know about you, but I love avocados and I push the limits on how much I eat. I have noticed I can definitely tolerate more than the 1/8 avocado serving size recommended (previously) in the Monash app. Now I know the reason for that. The Monash FODMAP team (always dedicated to keeping the low FODMAP diet science current and accurate) recently re-tested avocados for FODMAP content and they made an interesting discovery. Avocados, a food analyzed over 15 years ago when the diet was initially developed, surprisingly are not high in sorbitol as previously thought. They are high in a unique sugar polyol called perseitol.
Perseitol, unique to avocados, behaves similarly to sorbitol in the gut. More study of this unique polyol and its potential to trigger IBS symptoms is needed so Monash refrained from reclassifying avocados as low FODMAP for the time being. They did, however, increase the low FODMAP serving size so you can now confidently eat 1/4 - 1/3 of an avocado (up to 2.1 ounces) and that is still considered low FODMAP.
This discovery highlights the complexity of food science and emphasizes the importance of ongoing research in FODMAPs and IBS management. I am thankful Monash University continues to prioritize this science for all of our benefit!
For those missing avocados, I recommend doing your own tolerance testing to see if you truly can increase your avocado intake without triggering symptoms. Don’t know how to do that? I’m always here to help.
Stay tuned for more updates as the Monash team continues to delve into FODMAP science! Read the full article, including all the science, on the Monash Low FODMAP blog.
Looking for Low FODMAP recipes that include avocado? Head on over to my recipe club and type the word “avocado” in the search box. Voila! All my recipes that include avocado. You’re welcome. :-)
More Deliciously Low FODMAP™ tips and tools
What’s Fiber Got to Do With It?
Why is fiber so important for people with IBS and which kind is best
Fiber exists in multiple forms, each with distinct characteristics. For instance, some types of fiber readily dissolve in water, while others are easily broken down by gut microbes, and some remain relatively intact from entrance to exit!
The various characteristics of fiber determine how it works inside your body, what it does once it reaches your gut, and how well it’s tolerated when you have Irritable Bowel Syndrome (IBS). Experts like to divide fiber into two basic types: insoluble and soluble. Generally speaking, insoluble fiber doesn’t dissolve well in water, and soluble fiber does.
Why is fiber so important for people with IBS and which kind is best?
Regulating Bowel Movements: Fiber, especially soluble fiber, can help regulate bowel movements by adding bulk to stool, making it easier to pass. For those with IBS who experience constipation or diarrhea, fiber can help normalize stool consistency and frequency.
Relieving Constipation: Many people with IBS suffer from constipation, and fiber can help soften stool and promote regular bowel movements, making it easier to pass stool without straining.
Alleviating Diarrhea: While insoluble fiber can exacerbate diarrhea in some individuals with IBS, soluble fiber can help absorb excess water in the colon, which can help alleviate diarrhea and reduce urgency.
Supporting Gut Health: Fiber serves as a prebiotic, meaning it provides nourishment for beneficial bacteria in the gut. These bacteria help maintain a healthy gut microbiome, which is important for overall digestive health and may contribute to symptom relief in IBS.
Reducing Bloating and Gas: While some types of fiber can contribute to bloating and gas in individuals with IBS, soluble fiber is less likely to cause these symptoms. Additionally, fiber can help promote regular bowel movements, reducing the likelihood of bloating and discomfort associated with constipation.
Managing Weight: High-fiber foods tend to be more filling and can help you feel satisfied with smaller portions, which may aid in weight management. Maintaining a healthy weight is important for overall health and may help manage symptoms of IBS.
If you have IBS it's essential to be cautious about the types and amounts of fiber you consume, as some types of fiber can exacerbate symptoms.
Soluble Fiber Takes The Cake
Soluble fiber is gentle on the gut and helps regulate both diarrhea and constipation so it’s the type of fiber to look for when you have IBS.
Good sources of soluble fiber include:
Oatmeal
Barley
Quinoa
Flaxseeds
Chia seeds
Sunflower seeds
Macadamia nuts
Sweet potatoes (cooked and peeled)
Tofu (always choose firm tofu which is low in FODMAPs—not Silken Tofu which is higher in FODMAPs)
Coffee (YES! Coffee has fiber!) — I always recommend decaf coffee if you have IBS as caffeine is a gut stimulant and irritant
Low-FODMAP Fruits and Vegetables: There are many fruits and vegetables that are low in FODMAPs and are good sources of fiber. These include:
Berries (such as strawberries, blueberries, raspberries)
Oranges
Grapes
Pineapple
Kiwi
Broccoli
Avocado (keeping in mind 1/8 of an avocado is the low FODMAP serving)
Carrots
Cucumbers
Bell peppers
Spinach
Zucchini
Seeds and Nuts: Some seeds and nuts can be high in insoluble fiber, which may aggravate IBS symptoms. However, certain seeds and nuts are lower in insoluble fiber and can be well-tolerated, such as:
Pumpkin seeds (pepitas)
Sunflower seeds
Almonds (in small quantities)
Walnuts (in small quantities)
Gluten-Free Whole Grains: Some people with IBS find that reducing gluten in their diet can help alleviate symptoms. While not everyone with IBS needs to avoid gluten, incorporating gluten-free whole grains can be beneficial. Examples of gluten-free grains include:
Brown rice (white rice is not considered a whole grain)
Quinoa
Buckwheat
Millet
Fiber Supplements: If it's difficult to get enough fiber from food sources, you may consider adding a soluble fiber supplement to your daily routine. It's important to start with a small dose and gradually increase it to avoid triggering symptoms. Additionally, staying well-hydrated is crucial when increasing fiber intake to prevent constipation.
A couple of readily available soluble fiber supplements can be found on Amazon at the below links.
Acacia Senegal also known as gum arabic, acacia fiber, or acacia gum
You can also purchase fiber and all kinds of other supplements through the IBS Game Changer Dispensary directly with a 15% discount and free shipping on orders over $50.
If you follow my blog and use my recipes you’ll see I use Psyllium Husk as a stabilizer in some of my recipes such as my Amazing Seed Crackers. So, it’s not just a supplement!
It's essential to pay attention to your body's response to different foods and fibers and adjust your intake accordingly. It may be helpful to work with an IBS coach for personalized guidance and support while managing IBS symptoms. If that’s what you’re looking for, you know where to find me!
Have a question you’d like to have answered? Email me at hello@ibsgamechanger.com
More Deliciously Low FODMAP™ tips and tools
Anxiety and IBS: 8 Things You Can Do to Get Them Both Under Control
In this blog post, I’m addressing the intricate relationship between anxiety and Irritable Bowel Syndrome, exploring how they impact each other, and giving you some specific things you can do to get them both under control.
Anxiety, the pervasive feeling of worry and unease, is a common human experience. When it becomes chronic, however, it can manifest as a mental condition with far-reaching effects. In this blog post, I’m addressing the intricate relationship between anxiety and Irritable Bowel Syndrome, exploring how they impact each other, and giving you some specific things you can do to get them both under control.
Understanding Anxiety
At its core, anxiety is the response to a perceived threat, often related to an uncertain future event. Chronic anxiety, a mental condition characterized by excessive apprehension, is marked by real or perceived threats, leading to avoidance behaviors and physical symptoms such as increased heart rate and muscle tension. Anxiety disorders, including generalized anxiety disorder, panic disorder, PTSD, and social anxiety disorder, affect a significant portion of the adult population in the United States and around the world.
The Link Between IBS and Anxiety
Research indicates a clear link between IBS and anxiety. Approximately 44% of individuals with IBS also experience an anxiety disorder, compared to only 8% of those without IBS. Recent studies suggest shared genetic pathways between IBS and certain mental health conditions, emphasizing the close connection between the gut and the brain.
The Gut-Brain Connection
The gut-brain connection, a bidirectional communication system between the gut and the brain, plays a crucial role in regulating digestive functions, mood, and stress responses. Altered communication in people with IBS may lead to abnormal sensory processing, unpredictable gut functions, and visceral (organ) hypersensitivity, causing you to feel pain and other symptoms.
Breaking the Anxiety-IBS Cycle
The anxiety-IBS connection often creates a challenging cycle that people find difficult to break, leading to feelings of frustration and hopelessness. Treatment for IBS should include dietary and lifestyle changes, in addition to psychological interventions to address both physical and psychological aspects, and only in a few cases, medication.
Targeting the Gut-Brain Connection
Addressing both anxiety and IBS involves a holistic approach. Mindfulness, mind-body exercises, meditation, gut-directed hypnotherapy, and gut-directed Cognitive Behavioral Therapy (CBT) can target the gut-brain connection. On the mental health side, working with specialized professionals like therapists or psychologists helps address anxiety, while collaborating with a nutritional health coach can help you develop strategies for a healthier gut.
8 Things You Can Do Right Away to Help
Tackling the overlap between anxiety and IBS requires effort and multiple different strategies. While the journey may take time, gaining control over both aspects is possible, allowing you to live more fully. If you're navigating IBS and anxiety together, know that support and effective interventions are available, giving you a path toward a more balanced and fulfilling life.
Here are some things you can do right away that may help both anxiety and IBS:
Meditation/guided visualization for relaxation and stress/anxiety reduction, consider using the Nerva App from Mindset Health which is gut-directed hypnotherapy that has been studied and shown to be extremely effective.
If you drink caffeinated beverages, ween yourself off ASAP. Caffeine is a stimulant that in and of itself can cause anxiety. It’s also a gut-specific stimulant and those of us with IBS don’t need gut stimulation for the most part. I suggest switching to pure ginger tea which has excellent anti-inflammatory and antioxidant properties.
If you drink any sort of carbonated beverage (especially sugary or caffeinated sodas), ween yourself off ASAP. Carbonated beverages can cause GI irritation, gas, and bloating, and potentially exacerbate IBS symptoms. Switch to plain water (hot or cold).
If you drink alcohol, ween yourself off ASAP. Alcohol itself can cause anxiety (especially as a rebound after over-drinking) and it can irritate the GI tract, and change your gut motility (leading to diarrhea or constipation), it’s a diuretic that leads to dehydration (particularly bad if you suffer from constipation), it’s actually poison and your digestive system doesn’t need anything getting in the way of doing its good work.
Get some exercise even if it’s just around the house! If at all possible get outside in some sort of nature (even seeing just one tree!). If you can’t get out, then put some plants in your house so you can look at them while you walk around the house. This has been shown to reduce stress and anxiety almost as well as a walk in nature. If that’s impossible, even pictures of nature can be helpful! Just put them where you can look at them and do some visualization of being there in nature.
Journal – keep track of everything that goes into your body (food, drink, supplements, pills, all of it.). And document your symptoms every day too. This will help you start to see patterns that trigger flare-ups which in turn may trigger anxiety. You can use a blank journal or something like this Gut Health Journal. (If you sign up for coaching with me, I will send you my own journal—but really anything will work!)
A Low FODMAP diet can be key to reducing flare-ups and the associated anxiety that comes with those flare-ups. The diet is used to calm your system down and then, through a series of tests you conduct yourself, to determine your personal FODMAP sensitivity profile so you can reintroduce as many of the foods that once triggered you as possible. Want more information about the Low FODMAP diet? Check out my Low FODMAP FAQ.
Get connected with a health coach for guidance and support. This can help you get to resolution much faster than trying to do it all alone. If you’d like to have coaching time with me, feel free to schedule an appointment right here. We can do a 15-minute free intro and/or the full 8-week program so you can really make progress in getting your gut, your mind, and your life back on track.
Have a question you’d like to have answered? Email me at hello@ibsgamechanger.com
Selected sources:
Link note: This post may contain affiliate links for you to easily purchase items that are linked. I may earn a small commission from qualifying purchases but none of this costs you a thing so feel free to use the links! In addition, for some items, I have provided a special discount code for IBS Game Changers so be sure to use the code when you purchase an item to get the discount that has been arranged just for you.
More Deliciously Low FODMAP™ Tips and Tools
What You Need to Know About Cheese and the Low FODMAP Diet
Not all cheeses are created equal in terms of their compatibility with the low FODMAP diet. This article will help you make informed choices that align with both your preferences and your gut health.
Cheese comes in all shapes, sizes, flavors, and ages. Good cheese can be an amazing flavor enhancer in all kinds of recipes from savory to sweet. It’s also delicious on its own. But cheese has lactose and I’m on a low FODMAP diet. Doesn’t that mean it’s off-limits for me??
No, it does not! Read on to learn why and to understand how to identify the best cheeses for you to enjoy.
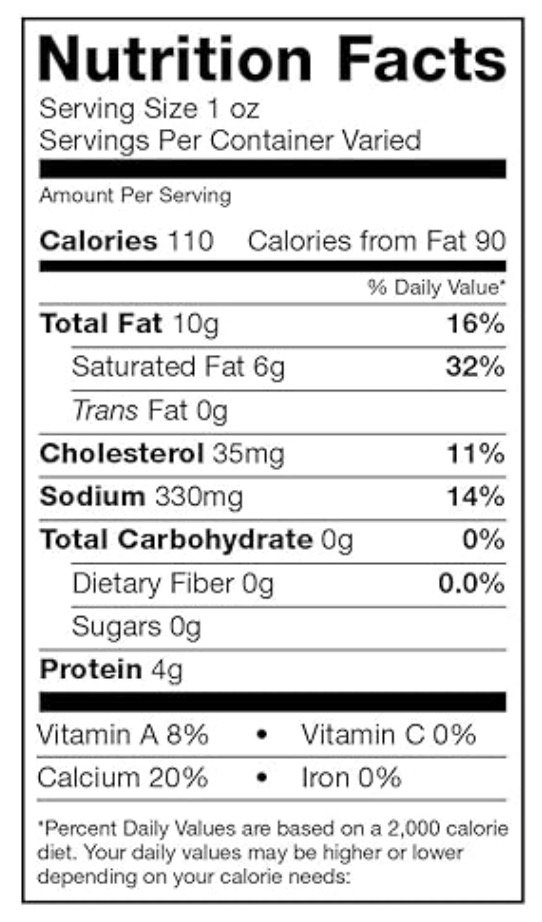
According to Monash University, a dairy product qualifies as low FODMAP if its lactose content is 1 gram or less per serving. This can be determined by assessing the Total Carbs, which includes both Carbohydrates and Sugars, as indicated on the cheese label. This is great to know because it means, whether a cheese has undergone lab testing or not, you can gauge its FODMAP content by examining the nutrition label.
If the Total Carbs on the nutrition label amount to 1 gram or less per serving, you can reasonably conclude that the dairy product is low FODMAP per serving. This aligns with Monash University's guideline of a low FODMAP serving containing 1 gram or less of lactose.
Individuals with IBS are often advised to adopt a "lactose-free" approach, leading to the exclusion of milk and cheese from their diets. However, it's important to note that a low FODMAP diet is not synonymous with being entirely lactose-free. (While some people with IBS may also be sensitive to dairy itself, this is a different issue.)
Nevertheless, not all cheeses are created equal in terms of their compatibility with the low FODMAP diet. This article aims to serve as a helpful guide, navigating you through the intricacies so you can make informed choices that align with both your preferences and your gut health.
Can You Eat Cheese on a Low FODMAP Diet?
Navigating the FODMAP content of cheese can be a bit intricate, but fear not – by the end of this article, you'll have a clear understanding of what you need to consider when selecting your cheese, whether it's undergone lab testing or not.
Numerous cheeses have been tested for their FODMAP content, and you can easily access this information through the Monash App on your phone. To make things even more straightforward, here's a list of cheeses that have been tested and confirmed to be low FODMAP in a serving size of 1.4 ounces (40 grams):
Brie
Cheddar
Feta
Goat cheese (such as Montrachet)
Havarti
Monterey Jack
Mozzarella
Swiss
What About Cheese That Hasn’t Been Tested?
Now, let's address the cheeses that haven't undergone lab testing, which includes some of my favorites, such as blue cheese, Gruyere, Jarlsberg, Parmesan, Fontina, and Provolone just to name a few. You are probably wondering if these cheeses are on the Low FODMAP menu.
The answer is: YES!
You absolutely can include these cheeses in your diet. As always, the key is to be a vigilant label reader and remember you’re looking for total carbohydrates and relative serving size.
It's worth noting that when you purchase cheese from a specialty cheese store, the cheese is typically cut to order and won't carry the nutrition label. What you learn from reading labeled cheese can be applied to these cut-to-order cheeses as well. Just keep serving sizes and weights in mind.
Decoding FODMAPs In Cheese
When it comes to cheese and FODMAPs, the primary concern is lactose. Learn more about Lactose and its effect on those of us with IBS in this excellent article written by my brilliant sister, Sarah Aitken, RN, MS, WHNP/FNP, MHP, NBC-HWC.
Here's the key to figuring out the serving size of untested cheese yourself: if the Total Carbohydrates and/or Total Sugars on the nutrition label amount to 1 gram or less per serving, you can confidently consider that the cheese is low FODMAP per serving. This aligns with Monash University's threshold for a low FODMAP serving regarding lactose, which is 1 gram per serving. So, by keeping an eye on these numbers, you can make informed choices about the FODMAP content in your cheese, ensuring a gut-friendly indulgence.
Read Those Cheese Labels!
Let's take a look at the label of traditional Danish blue cheese. Notice that the Total Carbohydrate per serving is listed as zero. Sometimes this may also be listed as < 1 (less than one). Zero does not mean there are zero carbs at any serving size but it DOES mean there is less than 1 gram of carbs per serving (which is 1 ounce in the case of most cheeses). This indicates that you can enjoy this particular blue cheese, adhering to the recommended serving size, even during the strict elimination phase of a Low FODMAP diet. And you may find, over time, you can tolerate larger serving sizes of cheese if you are not significantly triggered by lactose. (Need help figuring this out? Check out my Game Changer Program right here!)
In every case, when the Carbohydrates and Sugars—collectively referred to as Total Carbs—are under 1 gram per serving, they align with the low FODMAP designation established by Monash University, the gold standard for the FODMAP content of food.
If you come across blue cheese, Gruyere, or any other cheese in a recipe, a simple calculation of serving sizes will reveal whether the recipe falls within the low FODMAP category, specifically concerning the cheese. Whether you're referencing the nutrition label at home or doing this on the spot while shopping, a quick math check ensures you stay in tune with your FODMAP-friendly choices.
How Dairy Becomes Low FODMAP
Some dairy products are treated to reduce their lactose content, making them suitable for individuals with lactose intolerance or those following a low FODMAP diet. These products are labeled “lactose-free” even though most of them do contain lactose but they have been augmented with enzymes to break the lactose down as you eat it. Processes such as fermentation, aging, and specific enzyme treatments can also break down lactose before it even gets to your mouth.
As cheese ages, bacteria and enzymes used in the fermentation process actually consume some of the lactose in the cheese to fuel the fermentation. This results in lower levels of lactose in the final product. So, in general, the longer a cheese is aged, the lower the lactose in the cheese. Both soft and hard cheeses undergo distinct changes as they age and they share the commonality of containing low FODMAP amounts. Examples of aged cheeses include cheddar, Gruyere, Brie, Swiss, Parmesan, and so many more.
So, eat and enjoy every bite because you can!
Navigating Life with Irritable Bowel Syndrome: A Guide to Empowerment
Tips and Tools to help you navigate life while dealing with IBS
Living with Irritable Bowel Syndrome (IBS) can be a daily challenge, but it doesn't have to define your life. By approaching it from multiple directions and adopting a proactive and holistic approach, you can empower yourself to lead a fulfilling and balanced life. In this blog post, I’m sharing some practical tips and strategies to help you navigate the complexities of IBS and discover a sense of well-being.
Understand Your Triggers: The first step towards managing IBS is identifying your triggers. A great way to do this is to keep a daily diary to track your diet, hydration, exercise, stress, along with any symptoms you might be experiencing. This will help you pinpoint specific foods or stressors that may exacerbate your symptoms. Knowledge is power, and understanding your triggers is key to making informed choices.
Consult with Healthcare Professionals: Confirming your symptoms are related to IBS, vs something else, is a very important step. Once you’ve identified your most common triggers it’s always a good idea to consult with a gastroenterologist or your primary healthcare provider to discuss your symptoms, rule out other possible causes, and develop a personalized treatment plan.
Try a Low FODMAP Diet: Consider experimenting with a Low FODMAP diet, which restricts certain fermentable carbohydrates known to trigger IBS symptoms. It’s important, when trying any new diet, to keep your diary going by documenting your intake and your symptoms. It’s also important to ensure you're maintaining a balanced and nutritious diet. Lots of people identify a few things they can tolerate and they stick to just those things. This is not a good long-term strategy for managing IBS as you need great variety to ensure good health.
Prioritize Stress Management: Stress is a common trigger for IBS symptoms. Incorporate stress-reducing activities into your daily routine, such as mindfulness meditation, yoga, or deep breathing exercises. Establishing a consistent self-care routine can help you manage your stress levels and promote an overall sense of well-being, which in turn can diminish your IBS symptoms.
Stay Hydrated: Getting adequate hydration is crucial for digestive health. Ensure you're drinking enough water throughout the day (every day), as it helps maintain bowel regularity and supports overall digestive function. Build habits that help you maintain your hydration such as using a water bottle, or filling a glass in the kitchen that you drink every time you pass through.
Regular Exercise: Engage in regular physical activity, tailored to your comfort level. Exercise has been shown to alleviate IBS symptoms by promoting healthy digestion and reducing stress. Choose activities that you enjoy, whether it's walking, swimming, riding your bike, or doing some other form of gentle exercise. The most important thing, when choosing an exercise, is that you choose something you enjoy doing so you will do it regularly.
Build a Support System: Living with IBS can be emotionally challenging. Establish a support system of understanding friends and family, and consider joining an online community, such as my IBS Game Changer Community, where you can share experiences and get low FODMAP recipes and tips. Connecting with others who understand what you're going through can provide comfort and valuable insights.
Living with Irritable Bowel Syndrome is a journey, and it's essential to approach it with patience and self-compassion. By understanding your triggers, adopting a balanced lifestyle, and seeking support when needed, you can reclaim control over your life and thrive despite the challenges of IBS. Remember, you're not alone, and with the right strategies, living well with IBS is entirely within reach.
Need help on your journey?
More Deliciously Low FODMAP™ Tips and Tools
A Few IBS Game-Changing Tips for a Happy Holiday
From Mindful Munching to making Social Connections — here are some tips for a happy holiday!
As we all enjoy the holiday season, I want to extend warm wishes and a virtual hug to this incredible community of warriors who navigate the world of IBS with resilience and strength. Amidst the festive cheer, I understand the unique challenges the holidays can pose for those managing IBS symptoms. But fear not, I'm here to spread some joy and offer a few game-changing tips to make your holidays as enjoyable and stress-free as possible.
1. Mindful Munching: 'Tis the season of treats, and while indulging is part of the joy, I encourage mindful munching. Consider low FODMAP alternatives to your favorite holiday snacks, and savor each bite consciously.
2. Festive Flavors, Low FODMAP Style: Transform your holiday feast into a symphony of flavors that won't trigger discomfort. Explore some of my creative recipes that embrace the festive spirit while staying true to your low FODMAP lifestyle. Think roasted meats, flavorful herbs, and festive spices!
3. Sip Smart: Stay hydrated with gentle, soothing beverages. Opt for low FODMAP choices like peppermint tea or infused water with seasonal fruits (keeping an eye on FODMAP content, of course!).
4. Self-Care Amidst the Celebrations: Remember to prioritize self-care. Take breaks when needed, practice deep breathing, and find a quiet space to recharge. Your well-being is the best gift you can give yourself.
5. Connect and Share: The IBS journey can be challenging, but you're not alone. Reach out to this amazing community for support, tips, and shared experiences.
As we navigate the holiday festivities, let's celebrate the victories, big and small, that make us true IBS game changers. From me to you, may your holidays be filled with joy, delicious low FODMAP delights, and the warmth of connection.
Wishing you all a happy and healthy holiday season!
Warmly,
Katherine
More Deliciously Low FODMAP™ Tips and Tools
Halloween Candy Guide (What’s Low FODMAP and What’s Not)
What you need to know about eating Halloween candy
This time of year Halloween candy is everywhere you look. At work, at parties, at the checkout counter in your favorite store, even at the bank! And it’s tempting to enjoy snacking on a piece or two every place you go.
And let’s face it, at some point, you’re going to want to eat some Halloween candy!
If you are following a low FODMAP diet and Halloween is here. What do you do?
Instead of diving in and eating all of it with wild abandon, how about you do a little learning and planning so you don’t end up feeling terrible?!
Here are three rules to live by:
Don’t eat the candy at all those places I mentioned. You’ll just be stuffing it in your mouth because it’s there. Save your candy-eating for a time you can eat something you particularly like and you can take time to enjoy it.
Read the list below and stick to the low(er) FODMAP candies in the serving sizes recommended.
When you’re finished handing out candy to all the little neighborhood ghouls and goblins, toss it out or donate it. Don’t keep it around the house to “munch on” for days or weeks to come.
Keep it special. Keep it planned. And keep it to a minimum!
This list is excerpted from this post by FODMAP Every Day
Low(er) and High FODMAP Halloween Candy List
For the purposes of this list we are dealing with sweet candies and we feel fairly confident that no natural flavors were derived from onion or garlic, so a few of the candies listed below in the approved columns do contain natural flavors.
If you go rogue and start eating garlic jelly beans (yes, those are a thing), then all bets are off! Don’t do it.
Any candies that clearly list high FODMAP ingredients are on the high FODMAP list.
If you have a history with a particular ingredient, pay attention to your well-earned self-knowledge and stay away.
Serving Size Recommendations
Serving size recommendations are made by Vanessa Cobarrubia RDN as a guide and are based on the Monash University low FODMAP Diet App recommendations for serving sizes for individual ingredients.
As is always the case – we are not offering medical advice and you should always confer with your medical and healthcare team to ensure that you are following guidelines appropriate for your individual body’s needs.
Candy lists are below for your reference. See each list by clicking on the “+” sign to the right.
-
These are the candies we recommend (in alphabetical order by candy name) – in moderation, of course.
Atomic Fireballs: Practice moderation. Maybe 3 per serving.
Boston Baked Beans: Maximum 20 to 25 per serving.
Butterfingers: #7 on many favorite lists. These have some FODMAPs, but they are listed as less than 1% on the label. Start off with half a full-size bar or 1 to 2 fun size bars, or the equivalent of 3 to 4 bites.
Circus Peanuts: Practice moderation. Maybe 4 pieces max. Some say these are the most hated candy – but someone is eating them!
Conversation Hearts: Maybe 6 to 8 pieces max.
Dove Promises Silky Smooth Dark: Limit to 3 pieces (24 g total).
Dum Dums (lollipops): Limit to 4 to 5.
Haribo Gummi Bears: Limit to 15 gummi bears.
Haribo Sour Goldbears: Limit to 15 gummi bears.
Jolly Ranchers: Limit to 3 to 4.
Junior Mints: Limit to 12 mini mints.
Justin’s Dark Chocolate Peanut Butter Cups: Limit to 1 peanut butter cup (20 g) and increase to 2 peanut butter cups (if desired) based on personal tolerance.
Justin’s Milk Chocolate Peanut Butter Cups: There are no additional milk solids, milk, or lactose added in ingredients outside of the milk chocolate. Limiting to 1 peanut butter cup should keep milk chocolate in safe range.
Laffy Taffy: Limit to 3 mini pieces.
Lifesavers Peppermint and Wint-O-Green: Limit to 6
Marshmallows: Exclude any with high fructose corn syrup, inulin or other high FODMAP ingredients: For standard size limit to 4 to 5.
Mounds: Limit to ½ of a full size bar or 1 to 2 snack size bars.
Mr. Goodbar: Limit to ¼ of a full size bar or 1 fun size.
NECCO Wafers: Limit to 10 to 15 wafers.
Nerds: #6 on many lists. Limit to about 1 ½ tablespoons.
Peeps: These are marshmallows; see above. Limit to 3 to 4 peeps.
Reese’s Pieces: Limit to 20 to 25 pieces.
Skittles: #9 on many favorite lists. Limit to 15 to 20 skittles.
Smarties: Limit to 2 rolls.
Sno-Caps: Limit to 1 to 2 tablespoons.
Sour Patch Kids: #8 on many favorite lists. Limit to 6 to 8 pieces.
Swedish Fish: Limit to 2 to 3 pieces.
Sweet Tarts: Limit to 6 to 8 pieces.
-
We recommend that you do not eat these candies. Or, at least know what you are getting into.
Kit Kat: #4 on many favorite lists. Contain wheat flour, lactose, and dairy
Milk Duds: These are milk chocolate based, which is allowed in .5 ounce/15 g amounts, but also contain multiple milk products
Milky Way: These are milk chocolate based, which is allowed in .5 ounce/15 g amounts, but also contain additional milk products, lactose, and malted barley which is untested by Monash
Starbursts: Contain fruit juice concentrates, including apple.
Tootsie Rolls: Contain condensed skim milk and additional whey.
Twix: #3 on many favorite lists. Contain wheat flour, lactose, and dairy
-
For this category, Vanessa recommends trying a small piece to assess your own tolerances. Note that many of these come in “minis”, which might be a great place to start.
Almond Joy: These list milk products multiple times and we cannot be sure of the amount of lactose.
Dove Promises Silky Smooth Milk: These list milk products multiple times and we cannot be sure of the amount of lactose.
Heath Bar: These list milk products multiple times and we cannot be sure of the amount of lactose.
Hershey Bar: #10 on many favorite lists. These list milk products multiple times and we cannot be sure of the amount of lactose.
M & M’s: #5 on many favorite lists. We cannot be sure of lactose content. Try a few.
Mars Bar: These list milk products multiple times and we cannot be sure of the amount of lactose; also lists barley malt.
Nestlés Crunch: These list milk products multiple times and we cannot be sure of the amount of lactose; also lists barley malt.
Reese’s Peanut Butter Cups: #1 on many favorite lists. These list milk products multiple times and we cannot be sure of the amount of lactose.
Skor: These list milk products multiple times and we cannot be sure of the amount of lactose.
Snickers Bar: #2 on many favorite lists. These list milk products multiple times and we cannot be sure of the amount of lactose.
Three Musketeers: These list milk products multiple times and we cannot be sure of the amount of lactose.
Twizzlers: Contain wheat flour
More Deliciously Low FODMAP™ tips & tools
Exploring Metabolic Health: A Special Feature for Metabolic Health Day
20 Minutes prep • 25 Minutes cook • Low FODMAP • Serves 4
Metabolic health is a vital aspect of our overall well-being, yet it often remains overlooked. In recognition of Metabolic Health Day (October 10), in partnership with my sister, Sarah Aitken, RN, MS, WHNP/FNP, NBC-HWC, I’m delving into this crucial topic and addressing some of the most common questions:
What exactly is metabolic health?
Why is it so significant for our overall health?
Can you take steps to improve your metabolic health?
How is blood sugar interconnected with metabolic well-being?
Is it possible to gain insights into your metabolic health by utilizing continuous glucose monitoring?
And perhaps most importantly, can you reverse the consequences of years of neglecting your metabolic health?
Read on to discover the answers to these questions and gain a deeper understanding of the importance of metabolic health in our lives.
Curious about metabolic health? Wondering why it's essential? Ready to take charge of your well-being? You're not alone. Clients often ask these very questions, and the answers can pave the way to better health.
Understanding Metabolic Health
Metabolism fuels your body by converting the food you eat into energy for your cells. Optimal metabolic health ensures that these processes run smoothly. Metabolic health can be assessed through five key markers:
Blood sugar
Triglycerides
HDL (High-Density Lipoprotein)
Blood pressure
Waist circumference
If you're medication-free for these issues and these markers fall within the recommended ranges, your metabolic health is in excellent shape. But there's a sixth marker that's just as important – how you feel. When your metabolic health is on point, you feel good.
The Significance of Metabolic Health
Is metabolic health crucial? Absolutely! If you have three or more "worrisome" markers, you're at risk for diabetes, stroke, Alzheimer's, and heart disease. In fact, these markers can be used to predict or signify heart disease and likely prediabetes or diabetes.
A surplus of glucose in your bloodstream triggers oxidative stress and glycation. Poor metabolic health can lead to:
Low energy or energy fluctuations
Mental fog
Body pain
Fluid retention
Poor exercise stamina
Weight challenges
Widely varying moods
Skin issues
Fertility problems
Low libido or sexual issues
Susceptibility to infections
Improving Your Metabolic Health
Can you improve your metabolic health? Yes, you can! In the past, metabolic health was more of a given due to lifestyle and dietary choices. But as processed foods and snacking have become the norm, metabolic health has declined. In 2019, 88% of North Americans were deemed metabolically unhealthy. That means only 12% of us are metabolically healthy!
You can improve your metabolic health, often called metabolic fitness, by making daily choices that support your metabolic processes. Your diet, meal timing, sleep, stress management, physical activity, and more all play roles in this dynamic state of well-being. It's not an on/off switch; it's a daily continuum determined by your choices.
The Connection Between Blood Sugar and Metabolic Health
Glucose from your food is your cells' fuel. Insulin helps cells use glucose, but when cells aren't hungry for fuel due to frequent eating or highly processed foods, they become insulin resistant. This protective response keeps glucose out of cells, preventing them from overloading. When your blood sugar rises, it's a signal your cells are resisting insulin.
Can you tell something about your metabolic health by wearing a continuous glucose monitor (CGM)?
Absolutely! The glucose pattern of someone in poor metabolic health looks erratic, a roller coaster of variability.
They will likely see higher glucose peaks after eating high-starch foods. Their glucose may remain elevated for two or three hours after a meal or go up and down for several hours after eating. Morning glucose may be high, and/or the average glucose can be high.
Reversing the Damage of Poor Metabolic Health
Can you reverse the damage done by years of poor metabolic health? The answer is yes and no. Your organs and systems adapt to defend against glucose toxicity. This defensive mode can lead to various issues.
You can halt and even reverse some of this damage by:
Reducing the pressure on your liver, cardiovascular system, and pancreas
Lowering inflammation
Allowing for cellular cleanout
There's hope for a healthier future, and you have the power to optimize your metabolic health through daily choices.
Armed with this knowledge, you may feel you need help to make some changes to address your Metabolic Health. That’s where health coaching comes into play. If you have IBS and Metabolic Health concerns, learn about my program and set up a free consult with me and we can talk about how to tackle your issues! If you do not have IBS but you have pre-diabetes, weight management issues, or other metabolic health imbalances, then head on over to my sister site, Diabetes Game Changer. It might be just what you need to prepare yourself to have the best new year ever.
Here's to your best health and a thriving, resilient body.
Have a question you’d like to have answered? Email me at hello@ibsgamechanger.com
More Deliciously Low FODMAP™ tips and tools
Understanding Constipation: A Must for IBS Sufferers
Constipation: What is it? What are some common myths about it? What can you do about it?
What is it? What are some common myths about it? What can you do about it? And why are you looking at a picture of coffee?
For those of us with IBS, constipation is an important symptom to understand. If you're experiencing new or worsening constipation, seeking a gastroenterologist's evaluation, including a colonoscopy, is essential to rule out any underlying causes other than IBS. In this article written by my sister, Sarah Aitken, RN, MS, WHNP/FNP, NBC-HWC, for her Diabetes Game Changer Program, you'll find answers to most of the questions you might have about constipation.
Here’s the “Bottom” Line:
Whether you have IBS-C, IBS-D, or a combination of the two, IBS can manifest as constipation intermittently or all the time. I encourage you to read the full article for all the details.
Constipation has little to do with how often you poop and everything to do with how easy and comfortable your GI tract feels
Suffering from constipation does not mean you have an unhealthy diet
Hydration matters a lot
Moving your body matters, especially after meals
A regular and predictable eating routine helps
Medications could be the cause, so check them out with your provider
Increasing your intake of soluble fiber and avoiding processed foods might be all you need to do to fix the problem!
Still having issues and need customized and personalized support? Sign up for my IBS Game Changer Program and we can work together to get your gut on track.
More Deliciously Low FODMAP™ tips and tools
Tips for Navigating the Grocery Store Low FODMAP Style
A step-by-step guide to assist you in getting through the grocery store and coming out with all the low-FODMAP foods and ingredients you need.
Figuring out how to navigate a low-FODMAP diet can be challenging on its own. When you add the task of navigating the grocery store to find low-FODMAP foods and ingredients for enjoyable family meals, it can feel overwhelming and discouraging even before you’ve set foot in the store! To simplify this process, I've created a step-by-step guide to assist you in getting through the grocery store and coming out with all the low-FODMAP foods and ingredients you need.
Low FODMAP Grocery Shopping Made Easy
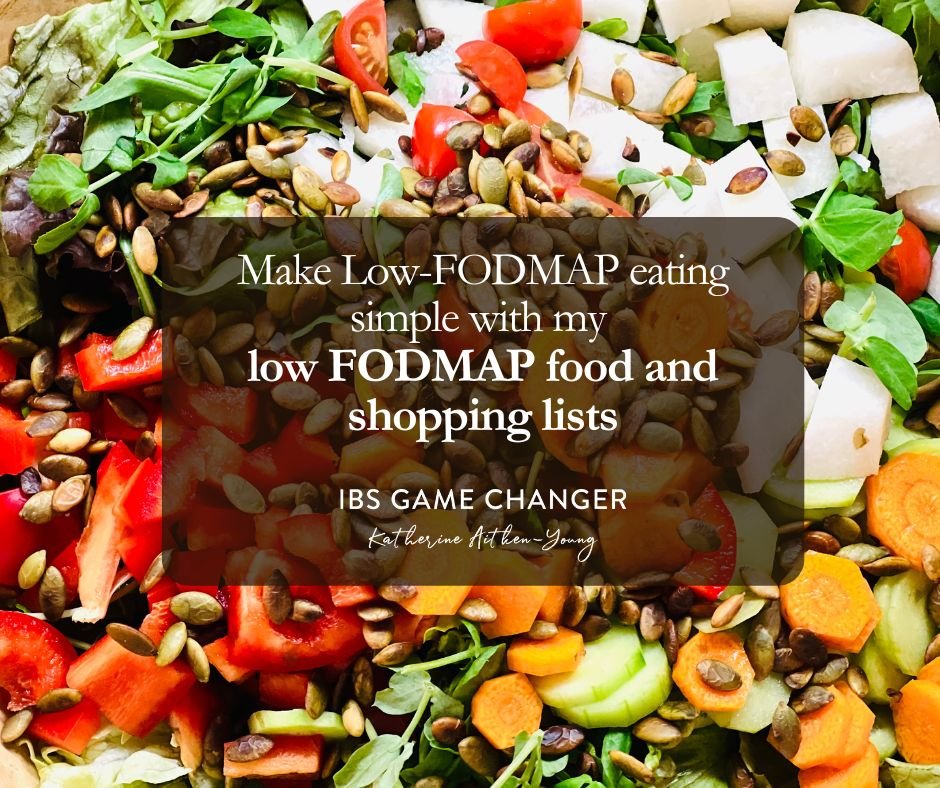
Educate Yourself: Familiarize yourself with the list of high and low FODMAP foods. You can use the Monash app or the Spoonful app for packaged foods, and you can use my food and shopping lists for easy/quick planning and buying.
Plan Your Meals: Before you go shopping, plan your meals and make a shopping list based on my low FODMAP recipes and meal plans. This will help you stay focused and avoid purchasing non-compliant foods.
Read Food Labels: When shopping, carefully read food labels for ingredients that are high in FODMAPs. Look out for ingredients like wheat, garlic, onion, high-fructose corn syrup, and artificial sweeteners. Avoid foods that contain these ingredients. Use the Spoonful app to scan barcodes and help you quickly assess FODMAP ingredients to watch for.
Stick to Whole Foods: The safest way to ensure you're getting low FODMAP ingredients is to focus on whole, unprocessed foods. Fresh fruits and vegetables, lean meats, fish, eggs, lactose-free dairy, rice, quinoa, and some gluten-free grains like oats are generally safe options.
Check for Certified Low FODMAP Products: Some brands now offer certified low FODMAP products. Look for the "Certified Low FODMAP" logo on the packaging, as this indicates that the product has been tested and approved as suitable for a low FODMAP diet. Some examples include Smoke N Sanity seasonings, salsas, and sauces; Fody Foods products, Green Valley and Good lactose-free dairy products, and others.
Avoid Onions and Garlic: Onions and garlic are common high FODMAP ingredients used in many processed foods and condiments. Instead, look for garlic-infused oils (the oil contains the flavor but not the FODMAPs) or use onion and garlic substitutes like garlic-infused oil or just the green parts of green onions, leeks, and spring onions.
Shop the Perimeter: In many grocery stores, the outside aisles of the store are where you'll find fresh produce, meats, dairy, and other whole foods. These are generally safer choices for a low FODMAP diet than all the processed foods on the inside aisles.
Beware of Hidden FODMAPs: Some foods that seem healthy may contain hidden FODMAPs. For example, certain fruits and vegetables in dried or canned forms, some gluten-free products, and certain sauces or marinades can contain high FODMAP ingredients.
Experiment and Keep a Food Diary: Everyone's tolerance to FODMAPs is different. After shopping for low FODMAP ingredients, be prepared to experiment with portion sizes and combinations of foods to determine what works best for your individual needs. Keeping a food diary can be helpful for tracking your symptoms and identifying trigger foods. The shopping lists linked in this article are excerpted from the journal I provide my coaching clients to track not only food and drink, but also exercise, stress level, bowel movements, and more.
Remember that while a low FODMAP diet can be beneficial for managing IBS symptoms, there’s more to it than that. Working with a healthcare professional who specializes in gastrointestinal health can be a real game changer. That’s why I created my 8-week program to provide just the right amount of guidance, education, and support to go from unpredictable and uncomfortable to predictable, comfortable, and in the driver’s seat! Take a look at the program here and read some of the success stories from program graduates.
Link note: This post may contain affiliate links for you to easily purchase items that are linked. I may earn a small commission from qualifying purchases but none of this costs you a thing so feel free to use the links! In addition, for some items, I have provided a special discount code for IBS Game Changers so be sure to use the code when you purchase an item to get the discount that has been arranged just for you.
More Deliciously Low FODMAP™ Tips and Tools
The Delicious Dimension: Exploring the Visual and Textural Joys of a Restricted Diet
While the nutritional content of food takes center stage, the way food looks and feels should not be underestimated.
When you’re limiting the selection of foods you eat for any reason, it’s important that the foods you do eat are as appealing and delicious as possible. That includes what your food LOOKS like and what it FEELS like when you eat it! Embarking on a restricted diet can be a challenging journey, often requiring meticulous attention to what you eat. While the nutritional content of food takes center stage, the way food looks and feels should not be underestimated. In this post, I’m digging into the significance of considering the aesthetics and textures of food when following a restricted diet and why this aspect matters for our overall well-being. I’ve included lots of links to delicious low-FODMAP recipes you can try when you’re ready to experience the many amazing things you can eat when following a low-FODMAP diet.
The Power of Presentation
A Feast for the Eyes: The old adage "we eat with our eyes first" holds true, especially for those on restricted diets. The visual appeal of food plays a crucial role in anticipation, satisfaction, and even the desire to consume the meal. When faced with dietary limitations, crafting visually appealing dishes can make each meal a delightful experience. Taking the time to chop some fresh herbs, grate some extra-flavorful cheese, or drizzle a little olive oil on the final dish can make all the difference. Try this Chicken Cobb Salad or Spring Roll Salad with Peanut dressing in my recipe club for example, or Better Than Takeout Sesame Chicken on my blog.
Emotional Fulfillment: Restricted diets can evoke feelings of deprivation and monotony. By putting effort into the visual presentation of meals, we transform our eating experience from a mere necessity to an emotionally satisfying ritual. A colorful and well-arranged plate can boost mood and elevate the overall enjoyment of the meal. Try my Super Simple Chocolate Lava Cakes or my Mushroom Gruyere Savory Bread Pudding, for example or any of the soup recipes in my recipe club.
The Crucial Role of Texture
A Multisensory Experience: Texture influences our perception of food more than we realize. The crunch of a fresh salad or the creaminess of mashed potatoes engages our senses, enhancing the dining experience beyond taste alone. This multisensory engagement becomes especially significant on restricted diets where the range of foods may be limited. Try my Crisp and Crunchy Chicken Salad, or my One Pan Thai Peanut Chicken and Veggies for example.
Appetite Stimulation: Texture can influence our appetite as well as our sense of satiation. Foods with varying textures stimulate our taste buds and appetite, making us more likely to enjoy and feel satisfied with a meal. For those adhering to specific dietary restrictions, incorporating diverse textures can make each bite more enticing. Try my Vegetable Chicken Stew, or my Chinese New Year Chicken Salad for example.
Mimicking Familiar Foods: On restricted diets, finding alternatives to favorite foods can be challenging. Texture can play a crucial role in replicating the experience of familiar meals. For example, creating a gluten-free pizza crust with a satisfying array of toppings can, not only mimic the texture of traditional pizza, but you might just find you like it even better than the original! This sameness with your old standards can provide a sense of comfort and normalcy. Check out this amazing Rosemary Mushroom Flatbread, or this BBQ Chicken Pizza with Bacon and Pineapple, or my Chocolate Cake with Umami Chocolate Frosting, in my recipe club for inspiration!
Expanding Culinary Creativity: Exploring new textures within the confines of a restricted diet can foster culinary creativity. Discovering how to use ingredients like nuts, seeds, and alternative flours to create crunchy crusts, velvety sauces, or chewy snacks can turn dietary limitations into an opportunity for innovation. In my recipes, I do my best to incorporate as much variety as possible—especially when it comes to plants as they play a vital role in keeping our gut biome healthy. Try my Umami Chicken and Butternut Squash Ramen, or my One Pan Chicken Arroz Caldo, for example.
Summing it all up
As we all experience our own IBS journey and the Low FODMAP diet that often accompanies that journey, keep in mind that food is not just sustenance—it's a sensory experience. The way food looks, feels, and engages our senses can significantly impact our relationship with our meals. By embracing the power of presentation and texture, you can infuse joy, anticipation, and a deeper connection with your meals. Crafting visually appealing dishes and experimenting with diverse textures can turn the challenge of eating a restricted diet into an opportunity to explore new horizons. So, let's celebrate the beauty and diversity of food, even within the boundaries of our dietary restrictions. After all, savoring a meal is not just about nourishment; it's about relishing life's sensory pleasures.
Have a question you’d like to have answered? Email me at hello@ibsgamechanger.com